
Understanding Clomid Resistance: Why Fertility Roadblocks Happen
If you’ve made it to this point, you’ve probably been through at least a few months of hope and anxiety. You take Clomid, maybe get those ultrasound checks, count down days, but nothing’s working. You’re not alone—about 15% to 25% of women diagnosed with ovulatory problems don’t respond to Clomid alternatives. The official medical term is “Clomid resistance,” and it can feel like hitting a brick wall, but it’s way more common than people think. What’s behind it? Most of the time, PCOS (polycystic ovary syndrome) is the main culprit, but sometimes high body weight, thyroid problems, or even certain genetic factors get in the way. Doctors usually define ‘resistant’ as not ovulating after 3–6 cycles on Clomid at its maximum recommended dose. If you’re here, you already know how deeply frustrating that can be.
It’s a weird place to be: you’re told Clomid is the “first-line” fertility pill, so when it doesn’t work, it feels personal—like your body missed the memo. But the truth is, medicine has a whole playbook for folks in your shoes. And to make things a bit brighter, some options have even better pregnancy rates than Clomid, depending on your own diagnosis. Before switching things up, it’s worth double-checking that you (or your partner) really did everything possible for Clomid to have a shot: like keeping a healthy weight, sticking to the schedule, making sure there’s no male-factor infertility, and getting thyroid/insulin resistance checked out. If those boxes are ticked and you’re still staring at a negative test, it’s time to get creative—and strategic.
Here’s a surprising fact: In a big U.S. trial, about 70% of women with PCOS ovulated on Clomid, but only about 20-25% actually got pregnant after several cycles. Why? Because ovulating isn’t always enough. Conditions like poor egg quality, thin uterine lining, or blocked fallopian tubes (which Clomid can’t fix) often hide in the background. A stepwise approach makes sense. That’s why a thorough checkup is a must. Make sure your doctor isn’t missing a more serious roadblock before switching treatments. Think of Clomid resistance not as an end, but as a sign it’s time for smarter, more targeted care.
If you’re worried about your fertility timeline, don’t stress too much. Advancing to a new phase after Clomid is standard. Around one in five women end up needing a different plan, and plenty of them go on to deliver healthy babies. The key: don’t keep taking Clomid in endless cycles. More isn’t always better, and it can actually thin your uterine lining and make things worse if you overdo it.
Let’s untangle what actually comes next. How do you know if you qualify for second-line options? What are the real success rates? How long should you try each one? Let’s lay out what real-world fertility journeys look like, so you can make sense of your own story without all the guesswork.
Second-Line Medical Treatments: What Really Works Beyond Clomid?
Now, if you’re moving past Clomid, doctors usually roll out “second-line” choices. These aren’t wild experiments—most are backed by major studies and trusted by top fertility clinics. The go-to options are letrozole (Femara), gonadotropin injections, and sometimes metformin (if you have PCOS or insulin resistance). Each one comes with its own pros, cons, and success rates.
Letrozole steals the spotlight here. It was originally used for breast cancer but has proven itself as a superstar in infertility solutions, especially for PCOS. Several studies, including a big Canadian one, found letrozole actually works better than Clomid for ovulation and pregnancy rates—especially if you’re overweight. Plus, it doesn’t thin the uterine lining, and the risk of twins stays lower. Most doctors start at 2.5 mg or 5 mg daily for five days, like Clomid, but some folks respond better to higher doses. It’s prescribed “off-label” for fertility, but don’t let that scare you; it’s safe and common.
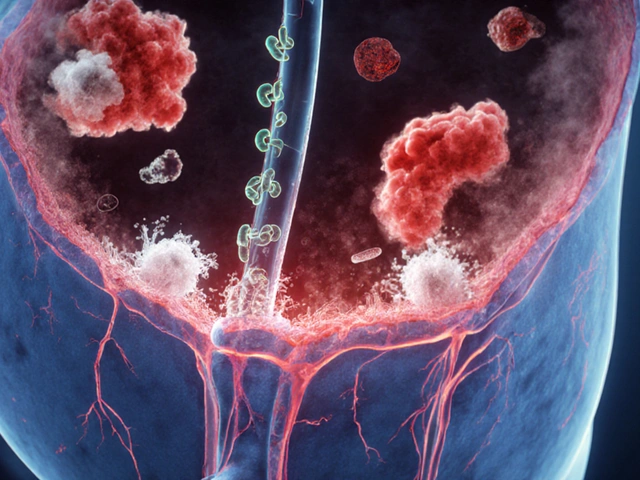
What if letrozole fails too? That’s where gonadotropins (FSH and LH injections) enter. These are basically the hormones your brain would send to your ovaries if it worked perfectly. Injections take daily commitment and a much closer watch—think more ultrasounds and more blood tests, plus a higher risk of twins or triplets. But success rates go up: People ovulating with gonadotropins get pregnant at rates of up to 50% per cycle. The biggest risk here is “over-response,” which can lead to ovarian hyperstimulation syndrome (OHSS), so only experienced clinics should prescribe them.
If you’re dealing with stubborn insulin resistance or have classic PCOS, metformin is sometimes added in before or along with fertility drugs. Several studies found that metformin improves response rates to both Clomid and letrozole, boosts live birth rates, and even reduces the risk of gestational diabetes once you’re pregnant. Doses start low and climb up over several weeks; stomach upset is pretty common at first, but most people handle it after a little while.
Here’s where it gets a bit more technical, but stick with me. Sometimes, your doctor might suggest combining pills (like metformin plus letrozole), or “step-up” protocols where you start with oral meds and move to injections only if those fail. And for people with clear signs of ovulation problems but no other fertility issues (especially if you’re under 35 and have been trying for less than three years), experts recommend three cycles on each second-line drug before moving to more advanced options like IVF.
If you want a much broader list—including newer drugs, herbal formulas, and comparison charts—check out these detailed Clomid replacement options. That link breaks down everything from prescription choices to supplements, with pros and cons for each.
Some real talk on what else to expect: Insurance can get tricky here. Pills like letrozole are cheap and often covered; injections and IVF can cost a lot if you’re uninsured. Ask your clinic for clear quotes before committing, and don’t be shy to discuss payment plans or shared risk programs. You’re not being a pest—being able to pay for ongoing cycles is a real-life factor in success. Another tip: clinics vary widely in their skill at managing complex protocols, so don’t be afraid to get a second opinion if you feel like you’re being pushed too quickly to IVF or aren’t getting enough monitoring during treatments.
Sometimes, second-line treatments include laparoscopy for women with PCOS who aren’t responding to medication. The procedure, called ovarian drilling, uses a tiny laser or needle to zap parts of the ovary and can sometimes restore ovulation in women for whom nothing else works. The effects usually last for a few months to a year, and pregnancy rates are about 30-50%. Like injections, this isn’t a step for everyone—surgery carries its own risks, so it’s reserved for very select cases.
At this point, the main medical workhorses are: letrozole, gonadotropins, metformin, and, rarely, ovarian drilling. If these all flop—or if you have blocked tubes or severe male-factor infertility—it’s time to think about IVF. But don’t panic; most folks trying their second or third fertility drug will succeed before you ever need test tubes or embryologists involved. The trick is always to track ovulation, pregnancy rates, costs, and (most of all) your own enthusiasm and mental health. If you feel burnt out, take a break; pregnancy is challenging enough without stress overload.
Lifestyle Tweaks, Complementary Therapies & Building Your Fertility “Toolkit”
Don’t underestimate the power of the stuff you do outside the doctor’s office. Lifestyle changes might sound boring after all the heavy-duty medicine talk, but the data is clear: small habits add up, especially if you keep at it for at least three to six months. Every major fertility society says getting to a healthy BMI (usually under 30 for women with PCOS) can double your chances of ovulating with or without drugs. Cutting just 5–10% of body weight, even if you’re not obese, can help bring back regular cycles. And if you’re on the slim side, adding weight can fix things, too—extreme exercise or strict low-calorie diets can tank ovulation as much as being overweight can.
Smoking, alcohol, and high caffeine intake (over 2-3 cups a day) all drop your chances. One study found women who smoke take up to twice as long to get pregnant as non-smokers, no matter what fertility pills they’re on. For the guys, quitting smoking and cutting down on alcohol bumps up sperm counts and motility, even if their test results look “normal.”
Supplements get a lot of hype, but a few actually have scientific backing. For women with PCOS or unexplained infertility, taking myo-inositol (2–4 grams daily) has been shown, in several real-world trials, to restore regular cycles and even boost Clomid and letrozole success by about 40%. Vitamin D (if you’re deficient), omega-3s, and coenzyme Q10 show promising data for egg quality, especially if you’re over 35. Be wary of “fertility teas” and unregulated herbs; they can interact with prescriptions or even mess with ovulation.
Acupuncture gets debated endlessly, but there’s definite evidence it can help with stress, anxiety, and—if you’re doing IVF—egg retrieval comfort. While it probably doesn’t boost ovulation directly, some couples swear by it for mental health and reducing cycle-related pain or bloating. Yoga and meditation work for stress as well, and one meta-analysis even showed higher IVF pregnancy rates for those who kept stress in check throughout the process. One thing’s for sure: mental health isn’t fluff. Research proves high levels of stress, depression, or relationship conflict can lower conception odds by up to 40%. Give yourself a break if you need one—it genuinely helps.
If you’re already cycling through meds but not ovulating, track everything: cycles, dosages, mood, energy, and symptoms. Bring this journal to every appointment. Doctors love data like that because it helps fine-tune your protocol and avoid repeating failed doses. There are some neat apps for it—Fertility Friend, Glow, and Ovia are top choices.
Male partner checks really matter. Between 25–30% of couples in fertility clinics discover a male factor was slowing them down, even with perfect female cycles. Get a semen analysis early, and encourage healthy habits—zinc, folic acid, and antioxidant-rich diets make odds better.
If you ever feel overwhelmed (and who doesn’t?), reach out to support groups. Resolve.org and mother-in-waiting communities on social media are loaded with people who “get it.” Peer advice can help you avoid rabbit holes and expensive treatments you might not need.
Now, here’s a quick trick: try to plan your next steps in 3–6 cycle chunks. That way, you always know when to try something new, instead of drifting along endlessly and burning out. Maybe you do three rounds of letrozole, add metformin, then try injections. If you’ve tracked everything and still aren’t pregnant, sit down with your doctor and map out IVF, egg donation, or other advanced plans (even if you’re not ready for them yet). Timelines empower you—in fertility, clarity is gold.
All the science, stats, and studies boil down to this: Clomid failing isn’t a personal failure. It just means your unique biology needs a more customized plan. There’s an entire arsenal of fertility treatments and real-world tweaks waiting. The couples who keep their options open and track their progress—medically and emotionally—give themselves the very best odds.
12 Comments
Michelle Thibodeau
July 18, 2025 AT 12:47 PM
Oh, I totally resonate with the rollercoaster of emotions when Clomid doesn't get the job done. It can feel like the ground just falls out from under you. This guide really does a beautiful job laying out the compassionate and practical routes forward, which is so important because the journey can be so isolating.
I particularly love how it doesn’t just shove more pills or injections down your throat but also emphasizes lifestyle - like stress management, diet, and even acupuncture for those open to it. The details about success rates were illuminating too; knowing you’re not alone or weird for your body responding differently is huge.
Does anyone have experiences with the alternative therapies mentioned? Like, how did you navigate those options emotionally and financially? Would love to hear stories to keep the hope alive.
Patrick Fithen
July 18, 2025 AT 16:33 PM
It’s fascinating how fertility treatments unfold. When Clomid fails, it’s like you’re left with a philosophical question — what next, and why did this path not succeed? The article’s approach to dissect second-line therapies alongside lifestyle choices is a beautiful intersection of science and human experience.
I wonder about the biopsychosocial model here—how much of infertility might be affected by external stressors or subtle hormone shifts influenced by lifestyle? The complementary treatments mentioned seem to open doors to holistic healing.
Curious to know, how do medical professionals decide on which second-line treatment to use? Is it just trial and error, or is there a predictive pattern based on individual patient history?
Michael Leaño
July 18, 2025 AT 20:20 PM
This article is such a beacon of hope for couples caught in the frustrating space when Clomid doesn’t trigger ovulation. I’ve seen a few friends go through this, and it’s heartening to have clear, practical guidance laid out so honestly.
The integration of both medical and lifestyle approaches acknowledges the multifaceted nature of fertility. It’s not just pills; it’s about the whole person. I think that message can’t be stressed enough during what is often a very isolating journey.
It’d be great to know more about the timeline for trying these second-line options — how long do folks usually wait before switching, and what are the emotional tools recommended to stay grounded during that wait?
Anirban Banerjee
July 19, 2025 AT 00:07 AM
This article provides a comprehensive yet succinct overview of second-line fertility treatments after Clomid failure, which is a common clinical challenge. The elucidation of alternatives such as injectable gonadotropins and letrozole is particularly valuable for patient education.
Further, the emphasis on lifestyle adjustments is commendable, as empirical evidence supports factors like weight management, nutrition, and stress mitigation in ovulatory function. However, it might benefit from elaborating on the criteria clinicians employ to select among second-line therapies, considering patient-specific variables.
A question arises regarding the accessibility and cost implications of these options in diverse healthcare settings, especially in less resource-rich environments. Any insights into navigating these barriers would enhance practical applicability.
Mansi Mehra
July 19, 2025 AT 03:53 AM
Whilst the article attempts to provide a guide on second-line fertility treatments, there are notable deficiencies in clarity that could mislead readers. The explanation of alternative medications lacks precise data on dosage and side effects, which are essential for informed decision-making.
The lifestyle recommendations, though well-intentioned, are presented in a cursory fashion devoid of substantiated research references. Emotive language should be balanced with factual rigor, particularly in medical contexts.
Furthermore, the statistical claims require proper citation to validate their accuracy. Without this, the article risks undermining its credibility, and consequently may engender unwarranted hope or confusion among patients.
Jagdish Kumar
July 19, 2025 AT 07:40 AM
My dear compatriots, this article is a veritable masterpiece in disseminating paramount information about fertility interventions beyond the oft-lauded Clomid. The precision with which alternative protocols, including the judicious use of gonadotropins and aromatase inhibitors, are detailed is most commendable.
Yet, I must express, with a modicum of theatrical lamentation, that the narrative demands more gravitas on the potential systemic ramifications of these therapies. The stakes could scarcely be higher for the hopeful denizens of the world.
Perchance a discourse on the biochemical pathways underlying these second-line options might elevate the erudition of this already exquisite compendium.
Aminat OT
July 19, 2025 AT 11:27 AM
Honestly, this whole ordeal with Clomid not working just rips you apart, you know? It's like your dreams being slapped in the face again and again. This article tries, but it’s all so clinical and cold, doesn’t it? Where’s the heart? The rawness of what folks go through?
And these "lifestyle tweaks" — are they even enough? Feeling like you have to overhaul your whole life just to maybe maybe conceive? It’s exhausting! I wish there was more talk here about the emotional chaos that’s not just a side note but the main storyline.
Anyone else feel like fertility clinics sometimes forget the human in the process? It’s more than numbers and meds.
Amanda Turnbo
July 19, 2025 AT 15:13 PM
Frankly, this article misses some crucial analysis of the efficacy rates and patient outcomes with second-line fertility treatments post-Clomid failure. It’s imperative that individuals seeking such guidance receive detailed, evidence-based information, rather than platitudes thinly veiled as advice.
Moreover, the purported "real stats" seem arbitrarily referenced without adequate methodological transparency. For the readers’ sake, comprehensive referencing and statistical robustness are non-negotiable in health communication.
It would also serve well to include potential adverse effects and contraindications of alternative therapies — an omission that borders on negligence.
Courtney The Explorer
July 19, 2025 AT 19:00 PM
Let me just say, it is absolutely critical that couples do not settle for subpar results with Clomid alone — moving swiftly to higher efficacy protocols is essential. Those who fail initial ovulation induction need urgent access to second-line therapies to maximize live birth rates.
The article’s attempt to present second-line options is appreciated but still lacking aggressive advocacy for immediate escalation to injectable gonadotropins where clinically appropriate. Time is a resource no one should squander in fertility treatment.
Furthermore, the text should have stressed more on the stringent monitoring required during these treatments to mitigate ovarian hyperstimulation syndrome risks. Safety cannot be compromised in the rush to conceive.
Ashleigh Connell
July 19, 2025 AT 22:47 PM
I find this article refreshingly gentle and thoughtful in addressing a topic that’s often drenched in clinical jargon and cold statistics. The encouragement towards incorporating lifestyle adaptations adds a holistic layer rarely discussed, which can be empowering for many.
That said, I wonder about the psychological impact the article lightly touches on — fertility struggles are as much emotional as physiological. Perhaps subsequent pieces could delve deeper into supportive practices like mindfulness or peer support groups alongside medical options.
Anyone here tried alternative routes like acupuncture or dietary shifts alongside their treatments? Would love to know how you balanced medical interventions with these approaches.
Michael Leaño
July 20, 2025 AT 02:33 AM
Thanks for everyone’s wonderful insights so far. I want to highlight that each person’s fertility journey is deeply personal, and while medical stats and treatments are essential, so is emotional resilience.
When Clomid didn’t work for my wife, we felt lost, but exploring second-line treatments with our doctor’s guidance and integrating stress-reduction techniques made a marked difference. Staying patient and hopeful, while being pragmatic, is a difficult but necessary balance.
If you’re reading this and struggling, remember you’re not alone and that expanding your fertility toolkit can open new doors worth walking through. Sending support and encouragement to all on this path.





Anthony Burchell
July 18, 2025 AT 09:00 AM
Honestly, Clomid not working is like the universe playing a bad joke, right? This guide breaks it down well, but I gotta say, sometimes docs push Clomid way too hard before moving on. The whole 'second-line' therapy thing sounds fancy, but how often does it actually work? Seems like a lot of trial and error before they hit the jackpot.
Also, lifestyle tweaks? Sure, but they’re generally so vague — like diet here, exercise there — it could mean anything. Anyone got real talk on what actually made a difference beyond the meds? And those "real stats" they mention, I wanna see those cold hard numbers, not just optimism.
Anyway, appreciate the article trying to give honest advice. Fertility stuff is a maze, and sometimes you need that no BS perspective, not sugarcoated hope. Thoughts?