
Fluoroquinolone Tendon Risk Calculator
Your Risk Assessment
This tool estimates your relative risk of tendon rupture when taking fluoroquinolone antibiotics based on factors mentioned in the article.
Your Risk Level
When you take an antibiotic like ciprofloxacin or levofloxacin, you expect to fight off an infection. You don’t expect to hear your tendon snap while walking to the mailbox. But for some people, that’s exactly what happens. Fluoroquinolones - a common class of antibiotics - have been linked to a serious, sometimes permanent, side effect: tendon rupture. And it’s not rare. It’s not theoretical. It’s happening in real people, often without warning.
What Are Fluoroquinolones?
Fluoroquinolones are synthetic antibiotics developed in the 1960s. They’re powerful. They work against a wide range of bacteria, which is why doctors still use them for serious infections like pneumonia, complicated urinary tract infections, and even anthrax exposure. Common names include ciprofloxacin, levofloxacin, and moxifloxacin. They’re sold under brand names like Cipro, Levaquin, and Avelox.
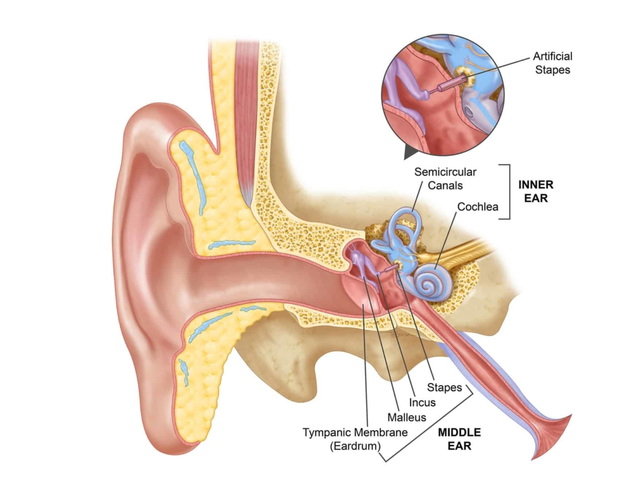
But their power comes with a price. Since the 1980s, doctors have noticed an unusual pattern: patients on these drugs were showing up with sudden, severe tendon pain - sometimes leading to complete rupture. The Achilles tendon, the thick cord at the back of the ankle, is hit hardest. In fact, nearly 90% of reported cases involve this one tendon.
The Real Risk: Tendon Rupture Isn’t Rare
Let’s talk numbers. A study of 6.4 million people in the UK found that those taking fluoroquinolones were more than four times as likely to develop tendinitis and twice as likely to suffer a full tendon rupture compared to those not taking them. That’s not a small risk. That’s a clear signal.
And it gets worse. If you’re over 60, the risk jumps. For people aged 60 to 79, the odds of rupture are more than six times higher. For those over 80? It’s over 20 times higher. Age isn’t just a number here - it’s a major red flag.
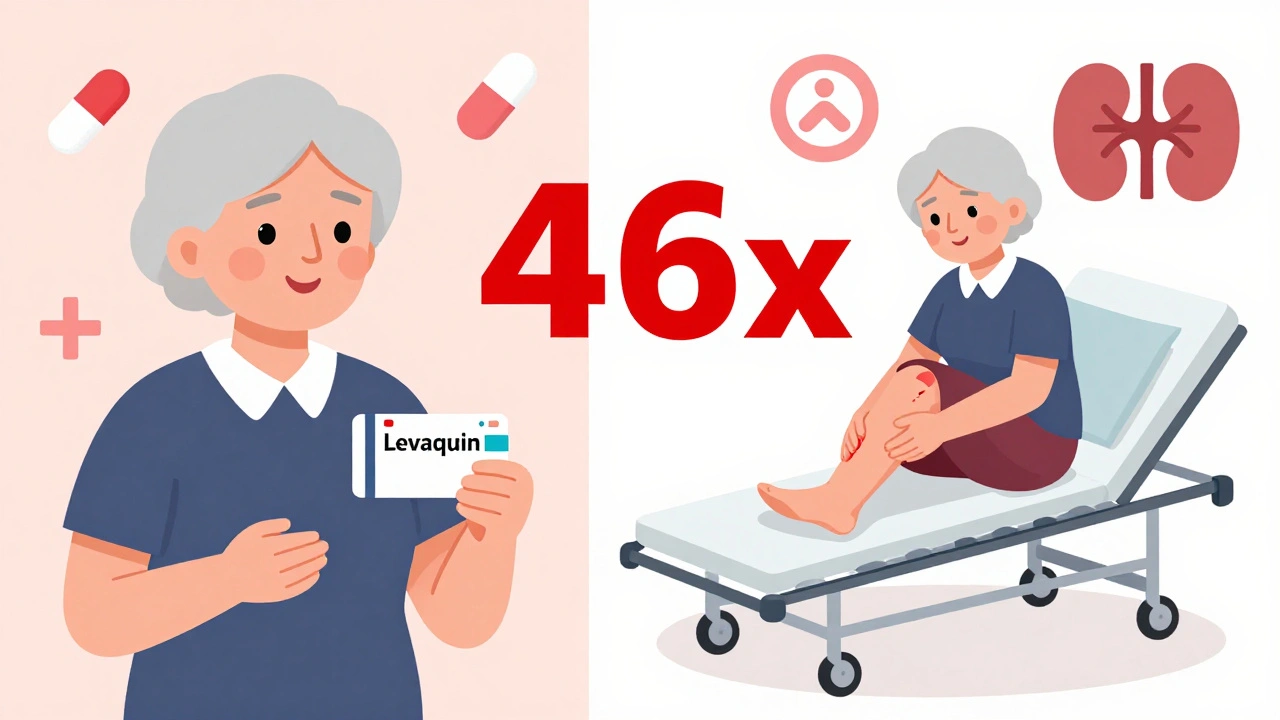
Another big factor? Steroids. If you’re taking prednisone or another corticosteroid - even a low dose - and you start a fluoroquinolone, your risk of tendon rupture increases by 46 times. That’s not a coincidence. That’s a dangerous interaction. The combination should be avoided at all costs.
Even more surprising? You don’t have to be active to get hurt. One case report described a man who ruptured his Achilles tendon while sitting down. No running. No jumping. Just standing up. The tendon gave out without warning.
When Does It Happen?
Most people assume side effects show up right away. Not here. The median time between starting the antibiotic and noticing tendon pain is just six days. But here’s the catch: symptoms can appear as early as 48 hours - or as late as several months after you’ve stopped taking the drug.
Half of all tendon ruptures linked to fluoroquinolones happen within the first week of treatment. In one documented case, pain started within two hours. That’s not a slow burn. That’s an alarm bell.
And because the damage can happen long after you’ve finished the pills, it’s easy to miss the connection. You might think your tendon pain is from aging, overuse, or an old injury. But if you took a fluoroquinolone in the past few months, it’s worth considering.
Why Does This Happen?
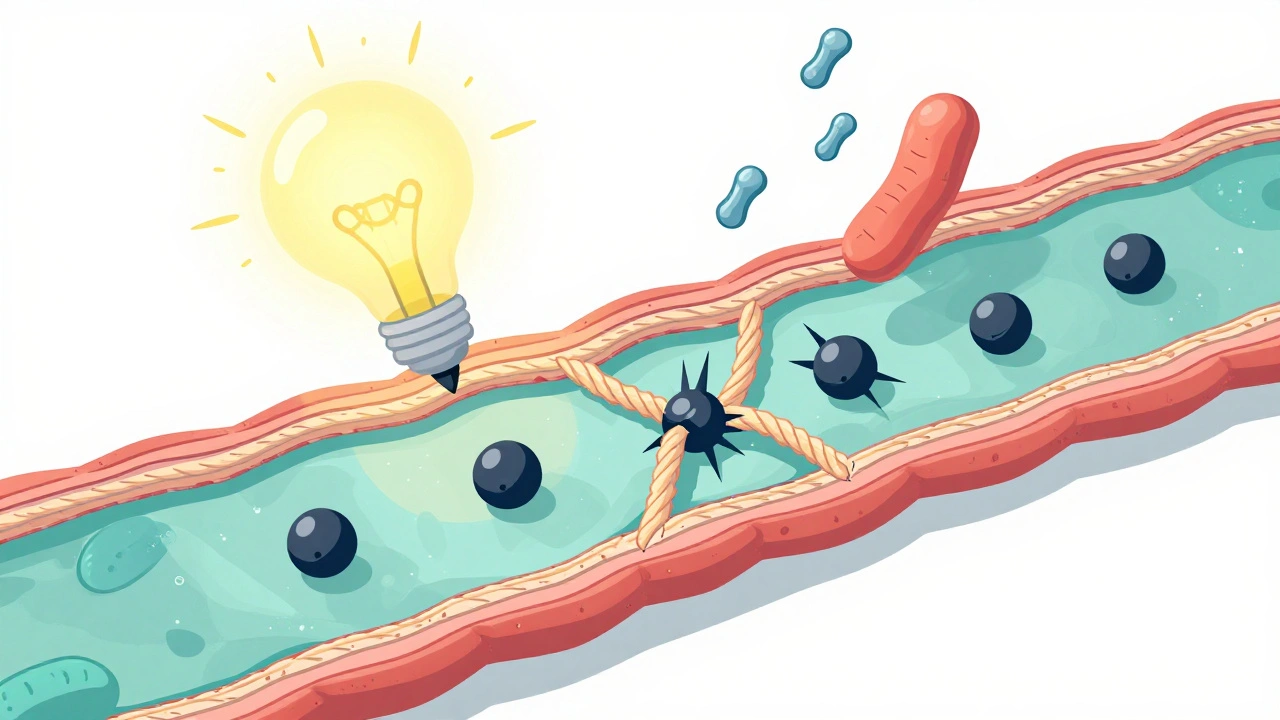
Scientists aren’t 100% sure, but they have strong theories. Fluoroquinolones don’t just kill bacteria. They also interfere with human cells - especially in tendons.
One theory: they trigger cell death in tendon tissue. Another: they mess with mitochondria, the energy factories in your cells, causing oxidative stress that breaks down collagen - the main protein that keeps tendons strong. They also pull calcium and magnesium out of the area, which weakens the signaling that keeps tendons healthy.
And why the Achilles? No one knows for sure, but it’s the thickest, most stressed tendon in the body. It’s under constant tension. When the tissue starts to break down, it’s the first to give way.
Who’s at Highest Risk?
It’s not random. Certain people are far more vulnerable:
- Age 60 and older
- Taking corticosteroids (oral or injected)
- Have kidney disease or are on dialysis
- Have diabetes
- Have had a previous tendon injury or rupture
- Are an organ transplant recipient
Women may also be at slightly higher risk, though the reason isn’t clear. Some studies suggest hormonal differences might play a role, but more research is needed.
And here’s the hard truth: if you have even one of these risk factors, fluoroquinolones should be your last option - not your first.
What Should You Do If You’re Prescribed One?
Don’t panic. Fluoroquinolones still have a place in medicine. For life-threatening infections, they can be lifesaving. But they should never be the go-to for a simple sinus infection, ear infection, or mild bronchitis.
Ask your doctor: "Is this the best choice for me? Are there safer alternatives?" If they say yes without explaining why, push back. There are plenty of other antibiotics - penicillins, cephalosporins, macrolides - that work just as well for most common infections.
If you’re already on one:
- Stop taking it immediately if you feel pain, swelling, or stiffness in any tendon - especially the Achilles, shoulders, or hands.
- Don’t wait for it to get worse. Early warning signs can be mild: a dull ache, slight warmth, or tightness.
- Avoid strenuous activity. Even walking too much can stress a weakened tendon.
- Don’t take steroids at the same time. Ever.
Once you stop the drug, symptoms may improve - but not always. Some people end up with chronic pain, limited mobility, or need surgery. Recovery can take months. In some cases, the damage is permanent.
What Are Doctors Doing About It?
Regulators have taken notice. The U.S. FDA added a black-box warning - the strongest possible - in 2008. They strengthened it again in 2013 and 2018. The UK’s MHRA and Europe’s EMA now restrict fluoroquinolones to only the most serious infections when no other options exist.
The Infectious Diseases Society of America now recommends fluoroquinolones be used as a third-line treatment - after safer antibiotics have failed.
And yet, in the U.S. alone, about 25 million fluoroquinolone prescriptions are written every year. Many are still given for conditions they shouldn’t touch.
What If You’ve Already Had a Tendon Injury?
If you’ve had a tendon rupture or severe tendinitis after taking a fluoroquinolone, you’re not alone. And you’re not imagining it. Document your experience. Talk to your doctor. Report it to your country’s adverse drug reporting system - like the FDA’s MedWatch in the U.S. or the MHRA’s Yellow Card system in the UK.
These reports help regulators understand how common this really is. They also help warn others.
And if you’re still on the drug and have symptoms - stop. Don’t wait for a rupture. Tendon pain is your body screaming for you to stop.
Final Thought: Antibiotics Aren’t Always the Answer
We’ve been conditioned to believe that if you feel sick, you need an antibiotic. But most colds, flu, and even many sinus infections are viral. Antibiotics don’t help. And when they’re overused, the risks - like tendon rupture - become real.
Fluoroquinolones are powerful tools. But like any powerful tool, they need to be handled with care. Don’t let convenience override caution. Ask questions. Push for alternatives. Your tendons - and your future mobility - depend on it.
12 Comments
Karl Barrett
December 7, 2025 AT 09:54 AM
The mitochondrial dysfunction hypothesis is the most compelling mechanistic model we have. Fluoroquinolones chelate divalent cations like Mg²⁺ and Ca²⁺, disrupting topoisomerase II activity in mitochondrial DNA, leading to ROS accumulation and collagen degradation. This isn’t just idiosyncratic toxicity-it’s a targeted assault on extracellular matrix integrity, particularly in high-tension tendons like the Achilles. The temporal window of risk extends far beyond dosing, which explains why patients don’t connect the dots.
Jake Deeds
December 7, 2025 AT 16:55 PM
People still take these like candy. I mean, really. You get a sinus infection, you go to the doctor, and they hand you a script like it’s a free candy bar. No wonder we’re all walking around with broken tendons. You want to be a hero? Don’t be the guy who took Cipro for a sniffle.
Alex Piddington
December 8, 2025 AT 07:38 AM
As a healthcare provider, I’ve seen too many cases. Fluoroquinolones are not first-line for uncomplicated infections. We have better, safer options. I always ask patients: 'Would you take this if you were my mother?' If the answer is no, we find another path. Your body isn’t a battleground-it’s a home. Treat it like one.
Ben Choy
December 9, 2025 AT 22:14 PM
I was on cipro for a UTI and got achilles pain on day 3. Stopped it. Pain went away. But I still get twinges sometimes. It’s been 2 years. I’m scared to even stretch. I didn’t know this could be permanent. I wish someone had told me before I swallowed the first pill.
michael booth
December 10, 2025 AT 12:12 PM
The epidemiological data is unequivocal. The FDA black-box warning, issued in 2008 and reinforced in 2013 and 2018, reflects a robust consensus among regulatory agencies and clinical experts. The risk-benefit ratio for fluoroquinolones in non-life-threatening infections is demonstrably unfavorable. Prescribing practices must evolve to reflect this evidence.
Libby Rees
December 10, 2025 AT 16:15 PM
I didn’t know this was a thing until my dad ruptured his Achilles after taking Cipro for a chest infection. He’s 72. No sports. Just walking to the kitchen. Now he walks with a limp. I’m never letting anyone I love take one of these without a fight.
Rudy Van den Boogaert
December 10, 2025 AT 22:06 PM
My sister took it for a UTI and had tendon pain so bad she couldn’t climb stairs. She went to her doctor and they told her it was just aging. She had to go to a rheumatologist to get the right answer. Doctors need to stop dismissing this. It’s not rare. It’s not just old people. It’s real.
Shofner Lehto
December 11, 2025 AT 11:48 AM
I’ve been a doctor for 25 years. I used to prescribe these freely. I don’t anymore. The data is too clear. The harm is too real. If you’re over 50, on steroids, or have any tendon history-don’t even consider it. There are 15 other antibiotics that work just fine. Don’t gamble with your mobility.
Emmanuel Peter
December 13, 2025 AT 01:24 AM
So you’re telling me someone broke their tendon just sitting down? Wow. That’s insane. I mean, if you’re dumb enough to take antibiotics for a cold, you probably shouldn’t be allowed to walk outside anyway. This is why people die from dumb choices.
Bill Wolfe
December 13, 2025 AT 10:00 AM
I’m sorry you all feel so entitled to your tendons. 🤦♂️ But let’s be real-most people who get this are already on 10 other meds, drink like fish, and sit on their butts all day. You think your Achilles is special? It’s just a tendon. Maybe if you exercised instead of scrolling TikTok, this wouldn’t happen. And no, I don’t care if you’re 70. You still owe your body better than this.
Dematteo Lasonya
December 13, 2025 AT 22:45 PM
I had a rupture on levofloxacin. Took 18 months to recover. Still can’t run. I reported it to MedWatch. No one ever called back. But I’m speaking up now because someone else needs to hear this before it’s too late. Don’t let them gaslight you. Tendon pain isn’t normal. Stop the drug. See a specialist. Your future self will thank you.





val kendra
December 5, 2025 AT 10:46 AM
I got tendon pain on levofloxacin and ignored it. Thought it was just sore from walking the dog. Next thing I know, I’m on the floor screaming. No warning. No warning at all. Stop taking it if you feel anything. Your tendons don’t come with a reset button.