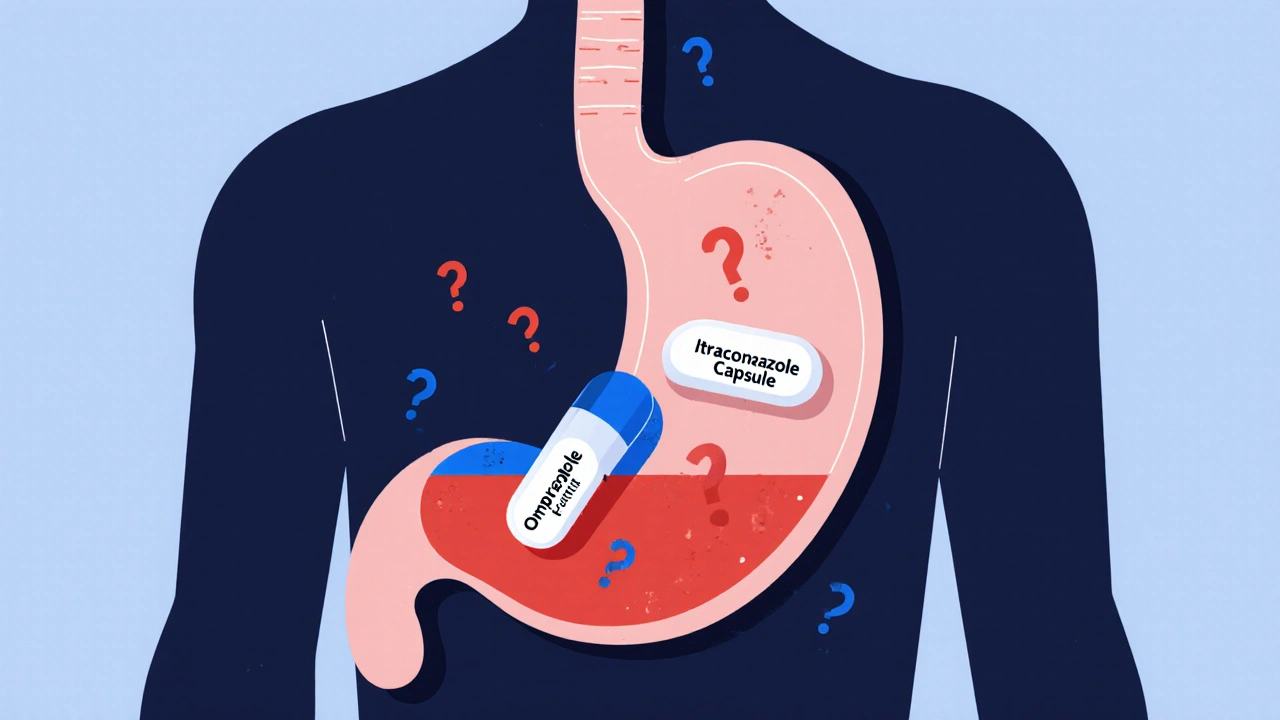
When you’re on a proton pump inhibitor (PPI) like omeprazole for heartburn and then get diagnosed with a fungal infection, your doctor might prescribe an antifungal like itraconazole. Sounds straightforward, right? But here’s the catch: omeprazole can seriously mess with how well that antifungal works - sometimes so much that the treatment fails.
Why Your Antifungal Might Not Work
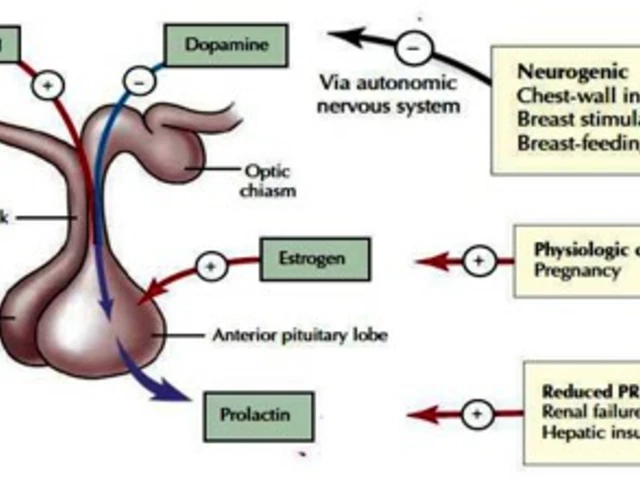
Proton pump inhibitors don’t just reduce stomach acid - they basically shut it down. They block the pumps in your stomach lining that produce acid, raising the pH from around 1-2 (super acidic) to 4-6 (nearly neutral). That’s great for ulcers, but terrible for certain antifungal drugs. Why? Because drugs like itraconazole and posaconazole are weak bases. They need acid to dissolve properly before your body can absorb them. If your stomach isn’t acidic enough, these drugs just sit there, undissolved, and pass right through your system. Studies show that when you take itraconazole capsules with a PPI, your body absorbs 50-60% less of the drug. That’s not a small drop - it’s the difference between healing and a worsening infection.Not All Antifungals Are Created Equal
This isn’t a problem with every antifungal. Fluconazole, for example, dissolves easily in water and doesn’t care about stomach pH. You can take it with your PPI and it’ll work fine. Voriconazole? It’s in the middle - about 22% less absorbed when paired with omeprazole. But itraconazole capsules? They’re the most vulnerable. Posaconazole delayed-release tablets? Also hit hard - 40% less absorption. Here’s the kicker: the liquid form of itraconazole (the solution, not the capsule) is designed differently. The drug is already dissolved, so it doesn’t need stomach acid. When taken with a PPI, absorption drops by only 10-15%. That’s why many hospitals now switch patients from capsules to solution when PPIs are needed.What About Other Acid Reducers?
H2 blockers like famotidine (Pepcid) or ranitidine don’t suppress acid as long or as deeply as PPIs. Studies show famotidine reduces itraconazole absorption by about 41%, compared to 57% with omeprazole. So if you absolutely need acid suppression and you’re on itraconazole capsules, switching from a PPI to an H2 blocker can help - but timing matters. Antacids like Tums or Maalox? They work fast and wear off fast. If you take them at least two hours before or after your antifungal, they won’t cause much trouble. But don’t mix them together - even a few minutes can throw off absorption.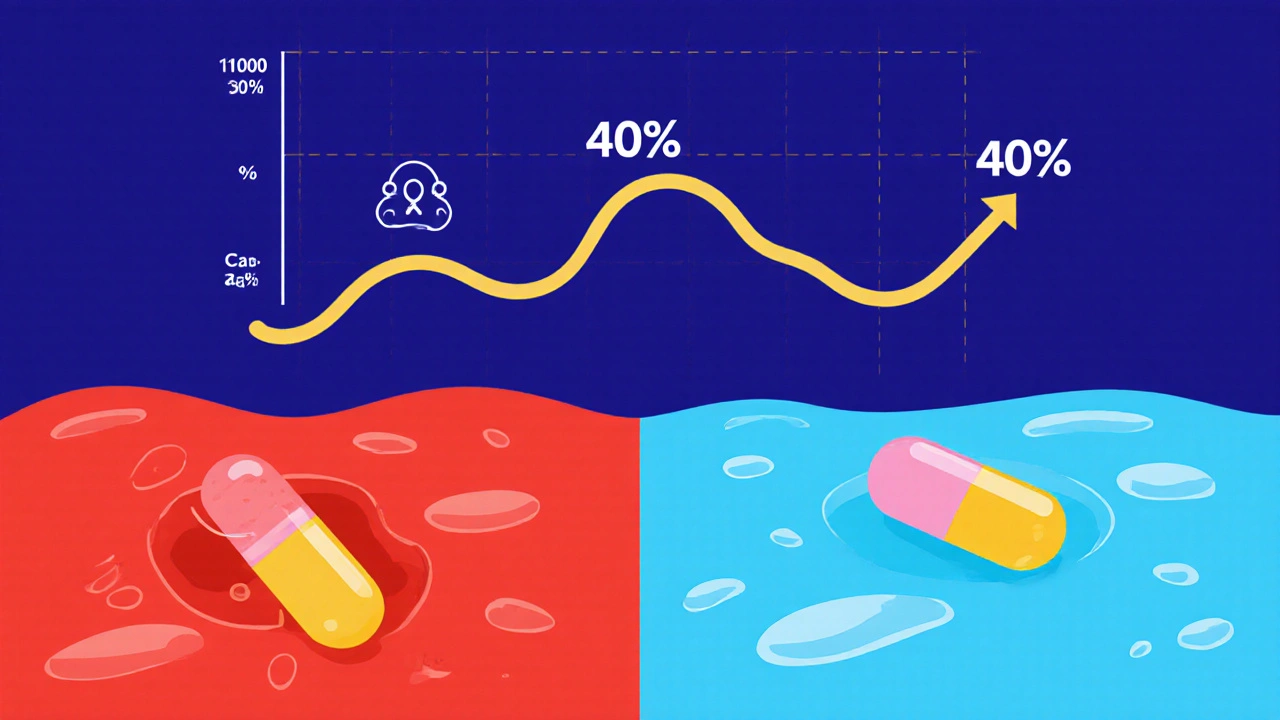
Real Cases, Real Consequences
In 2022, a survey of over 1,200 hospital pharmacists found that nearly 7 out of 10 saw at least one case a month where a patient’s antifungal failed because of a PPI. One case from Massachusetts General Hospital involved a man with chronic lung aspergillosis. His itraconazole blood levels were dangerously low - 0.3 mcg/mL - while the target is 0.5-1.0 mcg/mL. After switching from omeprazole to famotidine, his levels jumped to 1.7 mcg/mL. He recovered. Another patient, treated at MD Anderson, had invasive aspergillosis. His team kept the PPI but gave voriconazole two hours before it. That small delay made all the difference. These aren’t rare exceptions - they’re common clinical pitfalls.What’s Being Done About It?
In 2023, the FDA approved a new version of itraconazole called Tolsura. Unlike the old capsules, it’s formulated to absorb regardless of stomach pH. With a PPI, absorption drops by only 8% - a huge improvement. It’s not cheap, but for patients who need long-term PPIs and antifungals, it’s a game-changer. Meanwhile, researchers are looking at something unexpected. In lab tests, combining low-dose omeprazole with itraconazole actually killed resistant strains of Aspergillus fungus better than either drug alone. A clinical trial at the NIH (NCT05678901) is now testing whether this synergy can be used intentionally to treat drug-resistant fungal infections.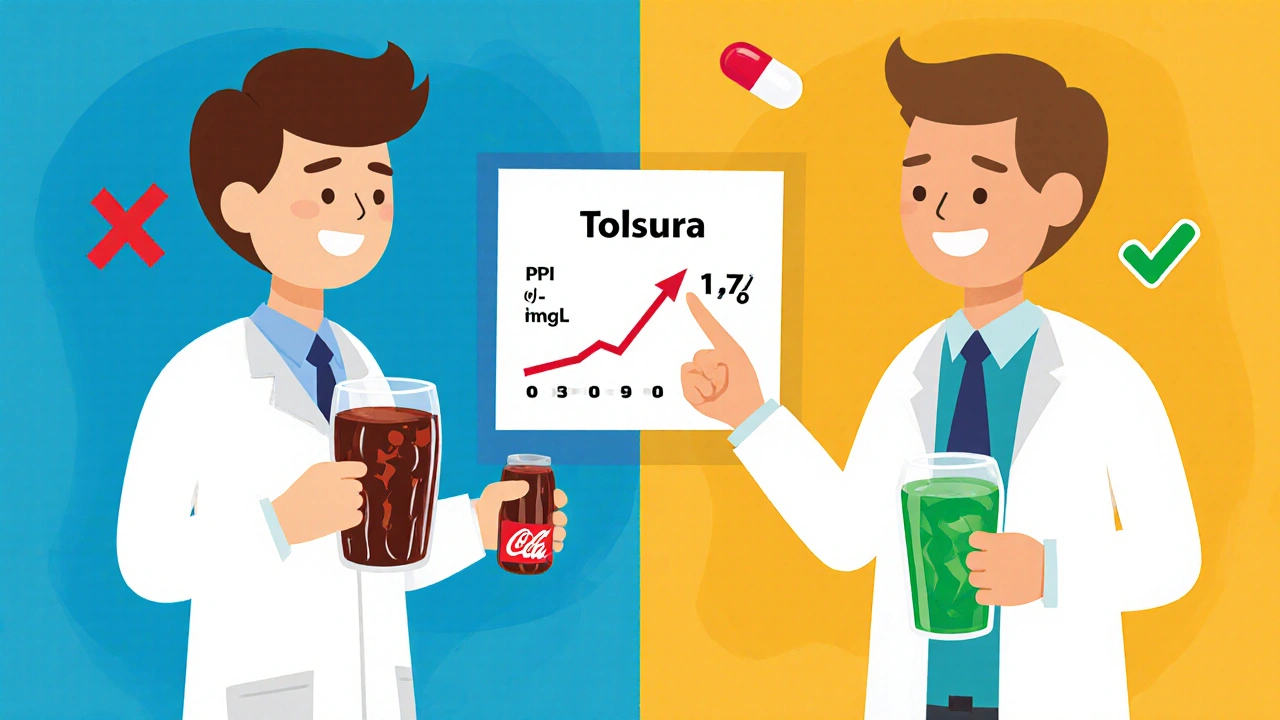
How to Manage This in Real Life
If you’re prescribed itraconazole capsules and you’re on a PPI:- Ask your doctor if you can switch to the liquid form of itraconazole.
- If you must keep the capsule, stop the PPI if possible - especially if you’re not at high risk for bleeding.
- If you can’t stop the PPI, switch to famotidine and take it at least 10 hours after your antifungal.
- For posaconazole tablets, take them with a glass of cola or another acidic drink. It helps.
- Never take antifungals and PPIs at the same time. Separate them by at least 2 hours.
- Ask for a blood test to check your antifungal levels - especially if you’re not improving.
Why This Matters More Than You Think
About 15% of U.S. adults take a PPI regularly. About 6% of hospitalized patients get a systemic antifungal. That means tens of thousands of people every year are getting these two drugs together - often without anyone checking if it’s safe. The cost? The U.S. healthcare system wastes about $287 million a year treating fungal infections that didn’t respond because the antifungal didn’t get absorbed. That’s not just money - it’s longer hospital stays, more IV drugs, and sometimes death. Pharmacists now have alerts built into electronic systems that flag this interaction. But those alerts only work if someone pays attention. Too often, the PPI is prescribed by one doctor, the antifungal by another, and no one connects the dots.What’s Coming Next
By late 2024, the Infectious Diseases Society of America and the American Gastroenterological Association plan to release new guidelines. They’ll have to balance two competing risks: the danger of fungal infections spreading versus the risk of stomach bleeding if you stop a PPI. For now, the message is clear: don’t assume these drugs play nice together. If you’re on a PPI and need an antifungal, ask: Which one? How is it absorbed? What’s the plan? Your life could depend on it.Can I take fluconazole with a proton pump inhibitor?
Yes. Fluconazole is highly water-soluble and doesn’t rely on stomach acid for absorption. Studies show no significant change in its levels when taken with omeprazole, lansoprazole, or any other PPI. You can take them together without adjusting timing.
Why does itraconazole capsule fail with PPIs but the solution doesn’t?
Itraconazole capsules contain solid drug particles that need stomach acid to dissolve before they can be absorbed. PPIs raise stomach pH, preventing dissolution. The solution form has the drug already dissolved in liquid, so it bypasses this step and gets absorbed directly in the intestines, regardless of stomach acidity.
Should I stop my PPI if I need an antifungal?
It depends. If you’re on a PPI for a serious reason - like recent GI bleeding or severe GERD with esophagitis - stopping it could be dangerous. Talk to your doctor. For mild heartburn or unnecessary long-term use, stopping or switching to an H2 blocker like famotidine is often safer and just as effective for the antifungal.
Is there a test to check if my antifungal is working?
Yes. Therapeutic drug monitoring (TDM) measures the level of antifungal in your blood. For itraconazole, the target range is 0.5-1.0 mcg/mL. If your levels are below that, your treatment may be failing - even if you’re taking the right dose. Ask your doctor or pharmacist if TDM is available.
Can I take antacids with my antifungal if I’m also on a PPI?
Antacids cause short-term pH spikes, so they’re less disruptive than PPIs. If you must use them, take them at least two hours before or after your antifungal. But don’t rely on them as a long-term fix - they won’t help if your PPI is still suppressing acid all day.
Are there new antifungals that don’t interact with PPIs?
Yes. Tolsura, a newer form of itraconazole approved in 2023, is designed to absorb regardless of stomach pH. It shows only an 8% drop in absorption with PPIs, compared to 50-60% for regular capsules. Voriconazole and isavuconazole are also less affected. Ask your doctor if switching to one of these is an option.
12 Comments
Summer Joy
November 21, 2025 AT 13:07 PM
So like… the FDA just approved Tolsura but it costs $800 a bottle? 😭 And we’re supposed to believe this isn’t Big Pharma playing us? PPIs are overprescribed, antifungals are expensive, and now we’re supposed to be grateful for a ‘better’ version that still needs a PhD to use properly? I’m just saying - if your doctor can’t figure out timing, maybe they shouldn’t be prescribing anything.
Nicole Ziegler
November 22, 2025 AT 16:52 PM
😳 I didn’t even know this was a thing. Just saved my mom’s life. She’s been on omeprazole for 5 years and just got antifungal for a rash. Now she’s switching to famotidine. Thank you for this. 🙏
Liam Strachan
November 23, 2025 AT 09:44 AM
Really appreciate this breakdown. I’m a pharmacist in London and we’ve been seeing more of these cases since PPIs became OTC. The liquid itraconazole switch is underused - we’ve had great success with it. Also, cola trick for posaconazole? Genius. Never thought of that. Thanks for sharing the real-world data.
Michael Fessler
November 24, 2025 AT 13:02 PM
just a quick note - if you're on itraconazole caps and a ppi, dont just stop the ppi without talkin to your doc. acid rebound is real. i've seen patients end up in er with esophagitis after going cold turkey. switch to famotidine or use the liquid. and yes, tdm is a game changer - ask for it. your dr might not bring it up but you should. also, dont forget to check for drug interactions with grapefruit juice. it messes with voriconazole too.
Jeremy Samuel
November 25, 2025 AT 09:59 AM
bro i think this is all just a scam. why would pharma make a new version of itraconazole? they just want you to buy more pills. also, cola? really? next they’ll say you need to drink energy drinks to absorb your meds. 😂
Ron and Gill Day
November 26, 2025 AT 05:20 AM
How is this even a topic? You’re telling me we need a 2000-word essay to explain that acid helps dissolve pills? This is like, Med School 101. I’m surprised anyone still prescribes itraconazole capsules in 2024. The fact that this is still a ‘problem’ is a national embarrassment. Also, who’s writing these guidelines? People who still use fax machines?
Matthew Peters
November 26, 2025 AT 12:16 PM
Wait - so the NIH is testing if low-dose omeprazole + itraconazole kills resistant fungus better? That’s wild. So the thing that breaks absorption… might actually be the secret weapon? That’s like using a wrench to fix a watch… then realizing the wrench is the only thing that can smash the broken gears. Mind blown. Anyone know if this trial’s open for participants?
Aruna Urban Planner
November 27, 2025 AT 16:01 PM
From a pharmacokinetic perspective, the pH-dependent solubility of weak bases is well-documented, but the clinical translation remains inconsistent across healthcare systems. In low-resource settings, therapeutic drug monitoring is often unavailable, making empirical substitution - such as switching to fluconazole or liquid formulations - the most pragmatic intervention. The structural distinction between capsule and solution formulations underscores the importance of pharmaceutical innovation in mitigating iatrogenic harm. Yet, systemic fragmentation in prescribing practices continues to undermine these advances.
Matthew Karrs
November 29, 2025 AT 15:50 PM
They’re hiding something. Why does the FDA approve a new version of itraconazole that costs 10x more, but never mention that PPIs were originally designed to be short-term? And why do all the studies come from hospitals that partner with drug companies? I’ve been on PPIs for 8 years. I’ve never had a fungal infection. Coincidence? I think not. Someone’s making money off fear.
Gerald Cheruiyot
November 30, 2025 AT 14:48 PM
we dont need more drugs we need better thinking
if your body cant absorb medicine because its not acidic enough maybe the problem isnt the medicine
maybe its the acid suppression
why are we fixing symptoms instead of causes
stop the ppi if you can
if you cant then yes switch to the liquid
but dont pretend this is just a dosing issue
this is a system failure
Dana Oralkhan
November 30, 2025 AT 21:24 PM
As someone who’s been managing GERD for 12 years and just started antifungal treatment last month - this post literally changed my life. I was about to give up because nothing was working. My pharmacist caught the interaction before I even knew it was a thing. We switched to fluconazole + famotidine at night. My rash is gone in 10 days. Thank you for writing this. I’m sharing it with my support group. You’re not just a writer - you’re a lifesaver.





Alyssa Torres
November 20, 2025 AT 22:44 PM
OMG this is LIFE-SAVING info. I had a friend who nearly died from aspergillosis because her doctor didn’t know about the PPI interaction. She was on omeprazole for years and got antifungals like it was candy. Turns out her blood levels were ZERO. Switched to fluconazole and the liquid itraconazole? She’s back to hiking and baking sourdough. Please, if you’re on PPIs, ask your pharmacist before taking ANY antifungal. This isn’t hype - it’s survival.