
Anticholinergic Burden Calculator
Check Your Medication Risk
Enter medications you're taking to calculate your total anticholinergic burden. Each medication contributes to your risk based on its ACB score.
Your Anticholinergic Burden Assessment
0
Low
Your current medications are at low risk for cognitive decline.
Medication Recommendations
Many people over 65 take medications for common issues like allergies, bladder problems, depression, or insomnia. What they don’t realize is that some of these everyday pills might be quietly damaging their brain. Anticholinergic drugs block acetylcholine, a key chemical for memory and thinking. And over time, that blockage doesn’t just cause dry mouth or constipation-it may be speeding up cognitive decline.
What Are Anticholinergic Medications?
Anticholinergic medications are a broad group of drugs that stop acetylcholine from doing its job in the brain and body. This can help with symptoms like muscle spasms, excessive sweating, or an overactive bladder. But it also slows down mental processes. Common examples include diphenhydramine (Benadryl), oxybutynin (Ditropan), amitriptyline (Elavil), and even some sleep aids and motion sickness pills.
There are about 100 of these drugs on the market-some prescription, many over-the-counter. And they’re everywhere. Around 10-15% of adults over 65 in the U.S. take at least one. That’s 15 to 20 million people. Many don’t know they’re taking something with strong anticholinergic effects. A 2021 survey found only 37% of primary care doctors routinely check for this burden in older patients-even though nearly 90% know it’s a risk.
How Strong Is the Link to Dementia?
The connection isn’t theoretical. Multiple large studies show a clear pattern. People who take anticholinergics for months or years have a higher chance of developing dementia. One major study using France’s national health database tracked over 1,000 people for more than a decade. Those who took the equivalent of more than 1,095 daily doses over time had a 49% higher risk of dementia compared to those who didn’t take any.
It’s not just one drug. It’s the total burden. Think of it like a scale: each medication adds a point. The more points, the higher the risk. Researchers use tools like the Anticholinergic Cognitive Burden (ACB) scale to measure this. A score of 3 or higher is considered high risk. Some drugs are stronger than others. Amitriptyline (an antidepressant) and oxybutynin (for bladder control) both score a 3. But trospium, another bladder drug, scores a 0-no anticholinergic effect.
Brain scans back this up. People on high-anticholinergic drugs show faster shrinkage in the hippocampus and amygdala-areas critical for memory. Their brains also use less glucose, a sign of reduced activity. One study found these patients lost 0.5-1.2% more brain volume each year than those not on these drugs.

Not All Anticholinergics Are the Same
It’s easy to assume all these drugs are equally dangerous. They’re not. The risk varies by class.
- Antidepressants (especially tricyclics like amitriptyline): Highest risk. Adjusted odds ratio of 1.29.
- Antipsychotics: OR 1.20.
- Bladder drugs (oxybutynin, solifenacin): OR 1.13-1.23.
- Antiparkinson drugs: OR 1.10.
- Antihistamines (diphenhydramine): High burden, but often taken short-term.
Here’s the kicker: trospium, a bladder medication, showed no increased risk. Mirabegron, a newer option for overactive bladder, has zero anticholinergic effect. So if you’re on oxybutynin for frequent urination, switching to mirabegron could cut your dementia risk without losing symptom control.
And it’s not just about the drug-it’s about how long you’ve been taking it. Short-term use (under a year) doesn’t show clear risk. But three or more years? That’s when the damage adds up. One 2023 study found long-term users had a 25% higher dementia risk.
What Does This Mean for Real People?
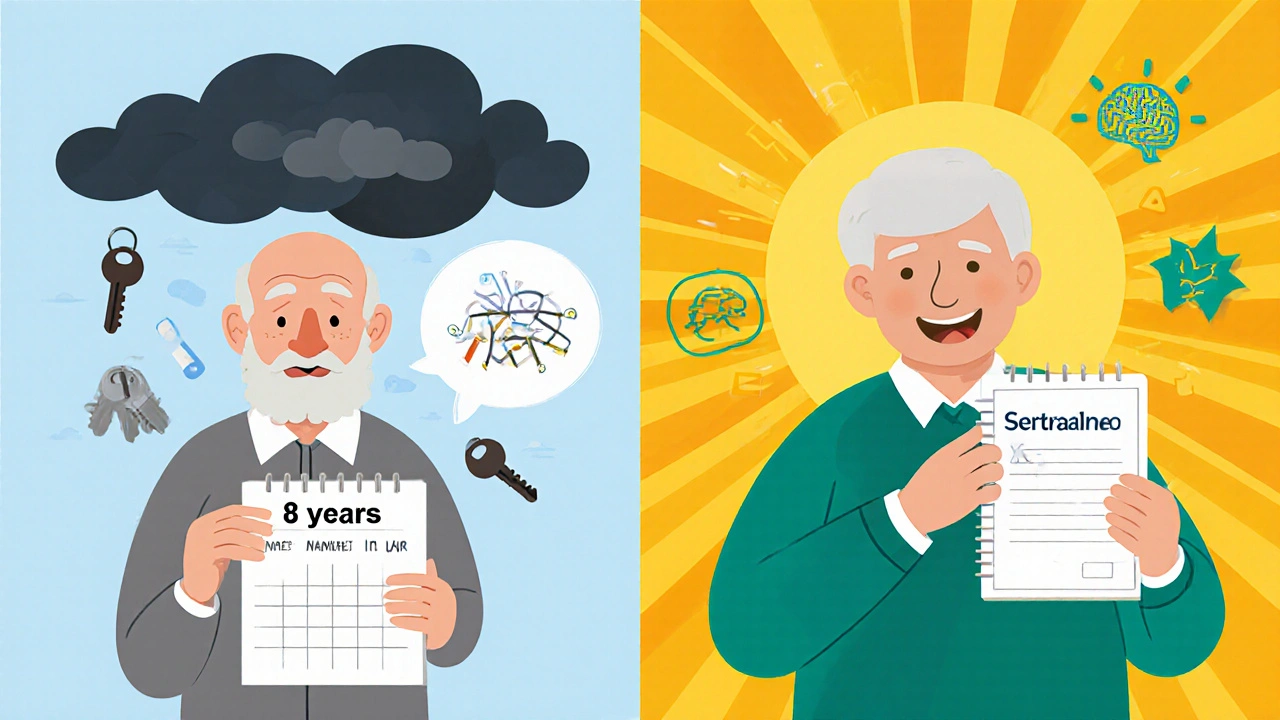
Real stories tell the truth better than data. One Reddit user shared that their mother took amitriptyline for nerve pain for eight years. Her memory test score dropped from 28 to 22 out of 30. After stopping the drug, her score stabilized-but never went back up. Another person in an Alzheimer’s support group said their confusion cleared up after switching from oxybutynin to a non-anticholinergic option.
But here’s the problem: most patients don’t connect their brain fog to their meds. On Drugs.com, 68% of oxybutynin users rate it as “excellent” or “good.” Only 22% mention memory problems. Why? Because the side effects are subtle. You don’t suddenly forget your name. You just start misplacing keys more often, forget names of friends, or feel mentally sluggish. You blame aging. Doctors blame aging. No one connects the dots.
And the labels? Only 42% of patient leaflets for anticholinergic drugs mention cognitive risk-even though EU regulations require it since 2017.
What Can You Do?
If you’re over 50 and taking any of these meds, here’s what to do:
- Check your list. Look at every pill you take-prescription and OTC. Write them down.
- Look up the ACB score. Search “ACB scale [drug name]” online. Many hospitals and pharmacies have free tools.
- Ask your doctor. Don’t just say, “Is this safe?” Ask: “Does this have anticholinergic effects? Is there a safer alternative?”
- Consider alternatives. For insomnia: try CBT instead of diphenhydramine. For depression: SSRIs like sertraline instead of amitriptyline. For overactive bladder: mirabegron instead of oxybutynin.
- Don’t quit cold turkey. Stopping suddenly can cause withdrawal-especially with antidepressants or bladder meds. Work with your doctor to taper off safely over 4-8 weeks.
The American Geriatrics Society’s Beers Criteria® already lists strong anticholinergics as drugs to avoid in older adults. Yet, they’re still widely prescribed. Why? Because they work. Bladder drugs reduce urgency. Antidepressants lift mood. Sleep aids help you rest. The problem isn’t the drugs-it’s the lack of awareness and better options.
The Bigger Picture
Dementia isn’t inevitable. About 35% of cases are linked to modifiable risks: high blood pressure, hearing loss, depression, diabetes, smoking. Anticholinergic use might be another major one. The Alzheimer’s Association estimates that cutting out unnecessary anticholinergics could prevent up to 15% of dementia cases each year-that’s over half a million people globally.
Change is coming. The FDA added stronger warnings to 14 anticholinergic drugs in 2020. The European Medicines Agency restricted some bladder drugs for elderly patients in 2021. The American Geriatrics Society launched a campaign to cut inappropriate prescribing by 50% by 2027. New drugs in development-like non-anticholinergic bladder treatments and antidepressants-are designed to avoid the brain entirely.
But until then, the power is in your hands. If you’re taking a medication that’s been on your shelf for years, ask: Is this still helping me-or is it slowly stealing my mind?
Can anticholinergic medications cause dementia?
Yes, long-term use of anticholinergic medications is strongly linked to an increased risk of dementia, especially in people over 65. Studies show that taking these drugs for more than three years can raise dementia risk by up to 49%. The risk builds over time and is tied to the total anticholinergic burden-not just one drug.
Which medications have the highest anticholinergic burden?
Tricyclic antidepressants like amitriptyline, bladder drugs like oxybutynin and solifenacin, and sedating antihistamines like diphenhydramine carry the highest anticholinergic burden. These are rated as level 3 on the Anticholinergic Cognitive Burden (ACB) scale-the strongest category. Avoid them if possible, especially if you’re over 50.
Is it safe to stop anticholinergic drugs on my own?
No. Stopping suddenly can cause serious side effects like increased heart rate, confusion, or worsening of the original condition. Always work with your doctor to taper off slowly. For antidepressants or bladder medications, a gradual reduction over 4-8 weeks is typically recommended to avoid withdrawal.
Are there safer alternatives to anticholinergic drugs?
Yes. For depression, SSRIs like sertraline or escitalopram have little to no anticholinergic effect. For overactive bladder, mirabegron is just as effective as oxybutynin but doesn’t affect cognition. For insomnia, cognitive behavioral therapy (CBT-I) works better than diphenhydramine and has no side effects. Ask your doctor about these options.
How can I check if my meds have anticholinergic effects?
Use the Anticholinergic Cognitive Burden (ACB) scale. Search online for “ACB scale” and the name of your medication. Many hospitals and pharmacy websites offer free lookup tools. You can also ask your pharmacist-they often have access to these databases. If your drug scores 2 or higher, talk to your doctor about alternatives.
12 Comments
Renee Ruth
November 14, 2025 AT 10:17 AM
Of course the system ignores this. Pharma makes billions off these pills. Doctors get paid to prescribe, not to think. And we’re just old people who ‘should be grateful’ for anything that helps us sleep. Wake up. This isn’t medicine-it’s slow poisoning with a prescription label.
My mom’s on oxybutynin. She’s been ‘forgetting things’ since 2018. Doctor said ‘it’s just aging.’ Guess what? She stopped it. Three months later, she remembered where she put her glasses. Twice. In the same day.
They don’t want you to know the alternatives. Mirabegron? Too new. CBT-I? Can’t be patented. SSRIs? Too expensive. So keep taking the cheap, dangerous crap. And thank them for it.
I’ve seen this play out too many times. The brain fog. The confusion. The way they stop laughing at their own jokes because they don’t remember why they were funny. It’s not dementia. It’s drug-induced brain rot. And no one’s holding anyone accountable.
They’ll say ‘correlation isn’t causation.’ But when 15 million people are on these drugs and their hippocampi are shrinking like dried fruit, and the same people are getting dementia at 2x the rate? That’s not luck. That’s a crime.
And don’t even get me started on the labels. 42% mention cognitive risk? That’s like putting a tiny ‘may cause cancer’ footnote on a pack of cigarettes. We’re being gaslit by the medical-industrial complex.
Don’t wait for your brain to go. Check your meds today. Not tomorrow. Today.
Samantha Wade
November 15, 2025 AT 15:39 PM
While the emotional tone of this discussion is understandable, it is critical to emphasize that the evidence linking anticholinergic burden to dementia is robust, longitudinal, and statistically significant across multiple peer-reviewed cohorts. The Anticholinergic Cognitive Burden (ACB) scale is not a speculative tool-it is validated in over 12 large-scale epidemiological studies, including the 2021 French cohort and the 2023 JAMA Neurology meta-analysis. Furthermore, neuroimaging data from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) confirms dose-dependent hippocampal atrophy in patients with ACB scores ≥3. The American Geriatrics Society’s Beers Criteria is not merely a guideline-it is a clinical imperative for geriatric prescribing. Patients over 50 should undergo a comprehensive medication reconciliation annually, with explicit review of ACB scores by pharmacists or clinicians trained in geriatric pharmacology. Discontinuation must be supervised, but avoidance of high-burden agents is not optional-it is preventative neurology.
Elizabeth Buján
November 17, 2025 AT 02:51 AM
i just read this and i cried. not because i’m scared, but because i finally get it. my dad took amitriptyline for 12 years. he used to tell the best stories. now he just stares at the wall. we thought it was ‘just getting old.’ turns out, it was the pill.
my mom switched to mirabegron last year. she’s 74. she’s laughing again. remembers my dog’s name. remembers what day it is. i wish we’d known sooner.
please, if you’re reading this and you’re on any of these meds-don’t panic. just ask. ask your doc. ask your pharmacist. say ‘is this hurting my brain?’ and don’t take no for an answer.
we deserve to remember our lives. not just survive them.
vanessa k
November 17, 2025 AT 14:51 PM
My aunt took diphenhydramine every night for insomnia. She started walking into walls. We thought it was dementia. Then she stopped the pills. Within six weeks, she could find her way to the bathroom again. No therapy. No meds. Just stopping the poison.
Why isn’t this on every prescription bottle? Why isn’t every doctor trained to check this? It’s not negligence-it’s profit.
manish kumar
November 17, 2025 AT 17:53 PM
As someone who has worked in pharmaceutical logistics in India for over 15 years, I can confirm that anticholinergic drugs are massively overprescribed in developing countries as well, often because they are cheap, available without prescription, and marketed aggressively under brand names that don’t even mention their active ingredients. In rural clinics, you’ll see patients given diphenhydramine for allergies, amitriptyline for ‘nervousness,’ and oxybutynin for ‘weak bladder’-all without any awareness of cognitive risks. The lack of pharmacist oversight and public education creates a perfect storm. Even in urban hospitals, doctors are overworked and often rely on formularies that prioritize cost over safety. The ACB scale is virtually unknown outside academic circles here. This isn’t just a Western problem-it’s a global silent epidemic. We need community health workers trained to flag these drugs, not just doctors. And we need public service campaigns in local languages, not just English medical journals. The data is there. The solutions are there. What’s missing is the will.
Nicole M
November 19, 2025 AT 09:45 AM
So… if I’m on a low-dose amitriptyline for migraines, should I panic? Or is it fine if I’ve only been on it for a year?
Arpita Shukla
November 21, 2025 AT 00:59 AM
You’re all missing the point. The real issue isn’t the drugs-it’s that people are living longer and the medical system hasn’t adapted. We’re treating 80-year-olds like 40-year-olds. Of course their brains are slowing down. It’s natural. You can’t just swap out every drug because someone’s memory isn’t perfect. And CBT-I? Try getting that covered by Medicare. Mirabegron costs $300 a month. Who’s gonna pay for that? You want to save brains? Fix the healthcare system first. Stop blaming pills for a broken model.
Benjamin Stöffler
November 22, 2025 AT 10:57 AM
And yet… we live in a world where a 78-year-old woman can be prescribed five anticholinergics simultaneously-each with a 3 on the ACB scale-while a 30-year-old with anxiety is given a 20mg daily dose of sertraline, which has an ACB score of 0. Why? Because the 78-year-old is ‘just getting old,’ and the 30-year-old is ‘a problem to be solved.’ The cognitive burden isn’t just chemical-it’s cultural. We treat aging as a disease to be medicated, not a stage of life to be honored. And in doing so, we are not preserving dignity-we are erasing it, one pill at a time.
Mark Rutkowski
November 23, 2025 AT 21:58 PM
There’s a quiet kind of grief that comes with realizing your brain has been slowly hollowed out by something you trusted. Not by fate. Not by time. By a pill you took because your doctor said it was safe. I’ve seen it in my mother. In my uncle. In my neighbor. We don’t scream about it because we’re too tired. Too confused. Too afraid to admit we’ve been betrayed by the very people sworn to heal us.
But here’s the truth: your mind isn’t yours anymore if you’re taking a drug that’s been quietly stealing your memories for a decade. And the worst part? You won’t know it’s gone until it’s too late.
So check your pills. Not because you’re paranoid. Because you’re alive. And you deserve to remember what it felt like to laugh with your grandchildren.
Ryan Everhart
November 25, 2025 AT 05:29 AM
So what you’re saying is… if I stop taking Benadryl, I might remember where I put my keys? Who knew? Next you’ll tell me drinking water helps with headaches.
David Barry
November 25, 2025 AT 17:31 PM
Let’s not pretend this is new. The anticholinergic dementia link was published in The Lancet in 2015. The FDA warned in 2020. The EMA restricted oxybutynin in 2021. And yet, here we are-still prescribing it like it’s aspirin. This isn’t ignorance. It’s negligence dressed up as tradition. The system doesn’t care if your brain shrinks. It cares if your insurance pays. And if you’re over 65? You’re a cost center, not a patient. The data is clear. The ethics are clear. The only thing missing? Accountability.






Andrew Forthmuller
November 13, 2025 AT 09:46 AM
My grandma took Benadryl for years. She forgot my name once at Christmas. Didn’t connect it till now.