For millions of people around the world, stomach pain, bloating, and unpredictable bowel habits aren’t just inconvenient-they’re life-limiting. If you’ve been told it’s "just stress" or "all in your head," you’re not alone. But here’s the truth: irritable bowel syndrome isn’t a mystery. It’s a real, measurable disruption in the communication between your gut and your brain. And understanding that connection is the key to real relief.
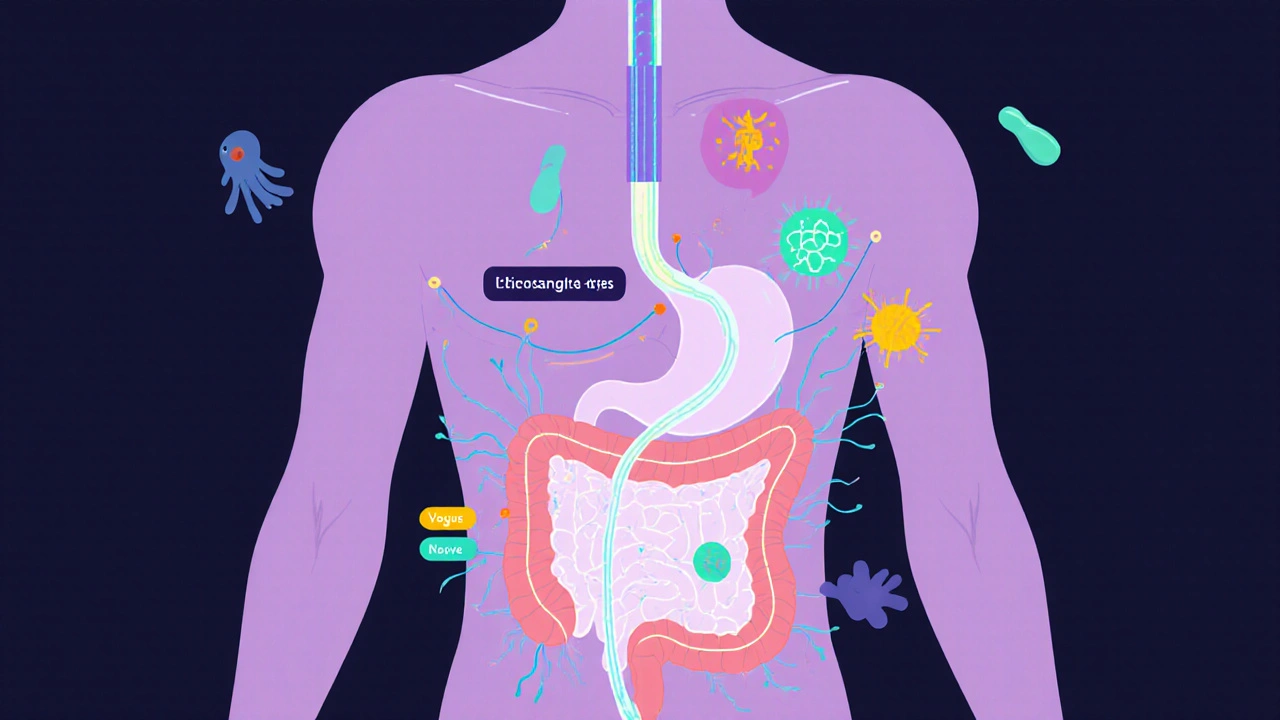
The Gut-Brain Axis Isn’t Metaphor-It’s Biology
For decades, IBS was treated like a plumbing problem. Doctors looked for infections, blockages, or inflammation. But when tests came back normal, patients were left confused-and often dismissed. The real issue? Your gut and brain are wired together. Not just loosely, but with a direct, two-way highway called the gut-brain axis.
This system includes your enteric nervous system (the "second brain" in your intestines), the vagus nerve, your stress hormones, immune cells, and even the trillions of microbes living in your gut. When this system gets out of sync, your gut starts sending wrong signals to your brain. Your brain, in turn, misreads those signals-turning normal gut movements into pain, or harmless gas into a full-blown crisis.
Brain scans show clear differences in people with IBS. The part of the brain that handles pain (the insula) is more active. The part that calms stress (the prefrontal cortex) is quieter. Your body isn’t broken-it’s miscommunicating.
Why Your Symptoms Don’t Match Your Test Results
IBS is diagnosed by symptoms, not scans or bloodwork. The Rome IV criteria say you have IBS if you’ve had abdominal pain at least once a week for three months, and it changes with bowel movements. That’s it. No inflammation. No tumors. No infection.
But here’s what most doctors don’t tell you: 76% of people with IBS feel constant discomfort, not just pain. Sixty to seventy percent also struggle with anxiety or depression-not because they’re "mental," but because the same brain circuits that process gut signals also regulate mood. Your gut isn’t causing your anxiety. Your brain’s misreading of gut signals is causing both.
And the numbers get even more telling. Ninety-five percent of your body’s serotonin-a key mood and gut regulator-is made in your intestines. People with diarrhea-predominant IBS (IBS-D) have up to 60% more serotonin in their gut lining. Those with constipation-predominant IBS (IBS-C) have too little. That’s not coincidence. That’s biology.
What’s Really Going On in Your Gut?
Your gut isn’t just a tube. It’s a living ecosystem. The microbes living there-bacteria, fungi, viruses-produce chemicals that talk directly to your brain. Studies show that people with IBS have different ratios of Firmicutes to Bacteroidetes bacteria than healthy people. These microbes don’t just digest food. They make short-chain fatty acids, neurotransmitters, and immune signals that shape how your brain feels about your gut.
One big clue? Immune cells in the gut of IBS patients produce less β-endorphin-the body’s natural painkiller. That means even mild stretching of the intestine can feel like cramping. Your gut isn’t more sensitive. Your brain just stopped listening to the signals telling it to calm down.
And then there’s food. Not because you’re allergic, but because certain carbs-called FODMAPs-ferment fast in your gut. They pull water in, swell your intestines, and trigger nerves that scream "pain!" to your brain. That’s why a bowl of beans or an apple can send you to bed, while someone else eats them without a thought.

The Best Ways to Reset the Gut-Brain Connection
There’s no magic pill. But there are proven ways to retrain your brain-gut system.
1. Low-FODMAP Diet
This isn’t another fad. In clinical trials, 50 to 76% of people with IBS saw major improvement. It works by removing foods that trigger fermentation and bloating-onions, garlic, wheat, dairy, apples, honey. You don’t cut them forever. You eliminate for 4-6 weeks, then slowly add them back to find your triggers. It’s hard. But 55% of people on Reddit’s IBS community say it’s the most effective thing they’ve tried.
2. Gut-Directed Hypnotherapy
Yes, hypnosis. But not stage stuff. This is a structured, science-backed therapy where you learn to calm your gut’s nervous system through guided imagery. In randomized trials, 70-80% of patients saw long-term relief-double the rate of standard meds. The effects last for years. It’s not mystical. It’s neuroplasticity: your brain learning to stop overreacting.
3. Targeted Probiotics
Not all probiotics help. Only specific strains do. Bifidobacterium infantis 35624 has been shown to reduce bloating and pain in 30-40% of users. It’s not a cure, but it’s a reset button for your gut microbes. Look for this exact strain on the label.
4. Neuromodulation
New tools like transcutaneous vagus nerve stimulation (tVNS)-a small device you wear behind your ear-are showing promise. In early studies, 45-55% of users reported less pain. It’s not FDA-approved yet, but it’s being tested in major hospitals.
5. Medications That Target the Axis
For IBS-D: Alosetron (a 5-HT3 blocker) helps 50-60% of women-but carries rare risks. For IBS-C: Prucalopride (a 5-HT4 agonist) improves bowel movement frequency in 45-55% of users. These aren’t your grandpa’s laxatives. They’re designed to fix the nerve signals, not just move things along.
Why Most Treatments Fail (And What to Do Instead)
Most people try antispasmodics, peppermint oil, or loperamide. They give short-term relief but don’t fix the root. And side effects? 63% of users report them. Many quit within three months.
The real problem? Doctors still treat IBS like a gut disease. But the fix isn’t in the intestines. It’s in the conversation between gut and brain.
Start with education. A 15-minute talk explaining the gut-brain axis changes everything. People who understand the mechanism are 30% more likely to stick with treatment-and see 25% better results.
Then go step by step: diet first, then hypnotherapy or probiotics, then meds if needed. Skip the random supplements. Don’t jump to colonoscopies unless you have warning signs like weight loss or blood in stool.
The Future Is Personalized
Scientists are now developing biomarker panels that measure your gut’s chemical signals-serotonin ratios, microbial metabolites, immune markers-to predict what treatment will work for YOU. One test, called VisceralSense™, is already 85% accurate in matching patients to effective therapies.
Big pharma is investing billions. New drugs like etrasimod are showing 52% symptom improvement in late-stage trials. The NIH has launched a $15 million project to map individual gut-brain profiles by 2030.
This isn’t science fiction. It’s the next chapter. And you don’t have to wait.
What You Can Do Today
You don’t need a miracle. You need a plan.
- Track your symptoms for two weeks: What you ate, stress levels, bowel habits. Look for patterns.
- Try a low-FODMAP elimination for 4 weeks. Use a trusted app like Monash University’s.
- Find a certified gut-directed hypnotherapist (search the American Society of Clinical Hypnosis directory).
- Ask your doctor about specific probiotics-not random brands.
- Stop blaming yourself. This isn’t weakness. It’s a biological misfire-and it’s treatable.
IBS isn’t your fault. But healing it? That’s your power.
Is IBS the same as IBD?
No. IBS (Irritable Bowel Syndrome) is a functional disorder-your gut looks normal but doesn’t work right. IBD (Inflammatory Bowel Disease), like Crohn’s or ulcerative colitis, involves actual inflammation, ulcers, and tissue damage. IBD shows up on scans and blood tests. IBS doesn’t. They’re completely different.
Can stress cause IBS?
Stress doesn’t cause IBS, but it makes it worse. When you’re stressed, your brain sends signals that slow or speed up your gut, increase pain sensitivity, and alter gut bacteria. That’s why flare-ups often follow big life events-job loss, breakup, illness. Managing stress isn’t optional-it’s part of treatment.
Why does my IBS change from diarrhea to constipation?
Because your gut-brain axis is unstable. IBS isn’t one thing-it’s a spectrum. Some people have IBS-D (diarrhea), others IBS-C (constipation), and many switch between them. This happens because your nervous system overreacts to different triggers-some foods, stress levels, or hormones. The same system that causes bloating can also cause urgency. It’s not random. It’s your brain misreading signals.
Are probiotics worth trying for IBS?
Only specific ones. Most store-bought probiotics won’t help. Look for Bifidobacterium infantis 35624-it’s the only strain with strong clinical evidence for reducing pain and bloating in IBS. Take 1 billion CFUs daily for at least 4 weeks. Don’t switch brands randomly. Consistency matters.
How long does it take to see results from gut-directed hypnotherapy?
Most people start feeling better after 4-6 sessions. Full benefit usually comes after 7-12 sessions, spaced weekly. The effects last-studies show relief continues for years. It’s not a quick fix, but it’s the most durable treatment we have.
Can IBS turn into cancer?
No. IBS does not increase your risk of colon cancer or any other cancer. It’s not a precancerous condition. But if you notice new symptoms like unexplained weight loss, blood in stool, or anemia, see a doctor. Those aren’t IBS signs-they’re red flags for something else.
Why do women get IBS more than men?
Hormones. Estrogen and progesterone affect gut motility, pain sensitivity, and serotonin levels. Many women notice worse symptoms around their period. That’s why IBS is 2-3 times more common in women. It’s not psychological-it’s hormonal biology.
Is the low-FODMAP diet hard to follow long-term?
Yes, the elimination phase is tough. 65% of people find it hard to stick to. But you don’t stay on it forever. The goal is to identify your triggers, then reintroduce foods you can tolerate. A dietitian can help you do this safely. Most people end up eating 70-80% of their favorite foods again-just not all at once.
13 Comments
Brandon Trevino
November 28, 2025 AT 19:26 PM
Let’s be precise: the gut-brain axis is a bidirectional neuroendocrine-immune signaling network with vagal afferents modulating central pain processing via limbic and cortical pathways. The Rome IV criteria are insufficient because they ignore microbiome metabolomic profiles and serotonin transporter polymorphisms.
Most FODMAP studies lack proper double-blinding. Also, hypnotherapy’s effect size is inflated by publication bias. You’re oversimplifying a complex neurogastroenterological disorder.
Maria Romina Aguilar
November 30, 2025 AT 18:33 PM
...I don’t know... maybe... it’s not the gut... maybe... it’s the wifi? Or the fluoride? Or... the government’s secret mind-control experiments in the water supply? I mean... look at the numbers... 76%... that’s too convenient...
Also... I read this one guy on a forum... who said... probiotics are just sugar pills...
...I’m just saying...
...maybe... it’s all in the head...
...but not in the way they say...
Hannah Magera
December 2, 2025 AT 06:19 AM
I’m new to this and honestly didn’t know any of this. I thought IBS was just ‘bad digestion.’
So the serotonin thing? That’s why I feel so anxious when my stomach hurts? It’s not me being dramatic-it’s my body talking?
Thank you for making this so clear. I’m going to try the low-FODMAP diet with my dietitian next week. I feel hopeful for the first time in years.
Austin Simko
December 2, 2025 AT 20:37 PM
They’re lying. The whole thing is a pharmaceutical scam. FODMAPs don’t exist. It’s glyphosate. They don’t want you to know. The WHO knows. The FDA knows. They’re hiding the truth. Probiotics are placebo. Hypnotherapy? Mind control. Watch the documentary. It’s all connected.
Nicola Mari
December 3, 2025 AT 20:37 PM
How can anyone take this seriously? You’re recommending hypnosis and probiotics like they’re medicine? What about discipline? What about willpower? I’ve had IBS for 20 years and I just stopped eating carbs. No magic. No science. Just self-control. You’re giving people excuses. Weakness is not a medical condition.
Sam txf
December 4, 2025 AT 10:16 AM
Wow. This is the most articulate thing I’ve ever read about IBS. Finally, someone gets it. The serotonin thing? Mind-blowing. I’ve been taking random probiotics for years-no wonder nothing worked. I’m getting Bifidobacterium infantis 35624 tomorrow. And I’m booking hypnotherapy. This isn’t woo-woo. This is science with soul.
George Hook
December 4, 2025 AT 19:25 PM
I’ve been living with IBS for 18 years. I’ve tried everything: elimination diets, peppermint oil, antidepressants, colon cleanses, acupuncture, even a raw food phase that lasted six months. Nothing stuck. But this-the gut-brain axis explanation? This is the first time I felt understood. Not just diagnosed. Understood.
I’ve spent thousands on tests that came back normal. No one ever told me my brain was misreading signals. They just said, ‘Drink more water.’
I’m not giving up. I’m starting with the Monash app and a certified hypnotherapist. I’m not broken. I’m just wired differently. And that’s okay.
jaya sreeraagam
December 4, 2025 AT 23:16 PM
Dear friend, I am from India and I have been suffering from IBS for 12 years. I tried Ayurveda, yoga, turmeric milk, fasting, and even a 7-day water fast. Nothing worked until I read this. The part about serotonin in the gut? That’s exactly what my Ayurvedic doctor tried to explain, but I didn’t understand.
I am going to try low-FODMAP with the Monash app. I also found a local hypnotherapist who specializes in digestive issues. I feel like I have a path now. Thank you for writing this with so much care. You are a light in the dark.
With love and hope,
Jaya
Katrina Sofiya
December 6, 2025 AT 08:07 AM
This is exactly what I needed to hear. I’ve been feeling guilty for years-like if I just tried harder, ate cleaner, meditated more, I’d be ‘fixed.’ But this? This isn’t about willpower. It’s biology. And that’s freeing.
I’m starting tomorrow. Low-FODMAP. Bifidobacterium infantis. And I’m calling my doctor about tVNS. I’m not waiting for the ‘perfect’ time. My body deserves this. Thank you.
kaushik dutta
December 8, 2025 AT 01:56 AM
Let’s contextualize this within the broader framework of neurogastroenterological pathophysiology. The gut-brain axis is not merely a neural conduit-it’s a dynamic, microbiota-modulated, immune-activated signaling network that integrates enteric neurotransmission with central autonomic regulation. The dominance of Firmicutes:Bacteroidetes ratios in IBS patients is corroborated by metagenomic analyses from the Human Microbiome Project (2012–2020).
However, the efficacy of low-FODMAP diets is confounded by nutritional inadequacy and microbiome dysbiosis exacerbation. Probiotics require strain-specific, dose-controlled, longitudinal administration-B. infantis 35624 is valid, but only in conjunction with prebiotic fiber modulation.
Neuromodulation via tVNS remains investigational. IBS is a systems-level disorder. Reductionist interventions will fail without holistic, personalized, multi-modal protocols.
doug schlenker
December 8, 2025 AT 03:07 AM
I’ve been reading this whole thing quietly. I didn’t comment because I didn’t think anyone would care. But… I have IBS. I’ve had it since I was 19. I’m 42 now. I’ve lost jobs because of it. I’ve canceled vacations. I’ve cried in bathroom stalls.
This isn’t just information. It’s validation.
I’m going to try the hypnotherapy. I’m going to get the right probiotic. I’m not going to feel ashamed anymore.
Thank you. For writing this. For not giving up on people like me.
Olivia Gracelynn Starsmith
December 8, 2025 AT 11:49 AM
Great breakdown. The serotonin-gut connection is critical and often ignored. Many practitioners still treat IBS as a digestive issue rather than a neurovisceral disorder. The low-FODMAP protocol is evidence-based but requires professional guidance to avoid malnutrition. Hypnotherapy data is robust-long-term remission rates exceed 70%. Probiotics must be strain-specific. tVNS is promising but not yet standard of care. Track symptoms. Be systematic. You’re not alone.




Denise Wiley
November 28, 2025 AT 12:54 PM
This post changed everything for me. I’ve been told it’s stress for years, but now I get it-it’s my brain and gut having a bad conversation. I started low-FODMAP last week and already feel less bloated. No more hiding after lunch.
Thank you for explaining serotonin in the gut. I didn’t know 95% of it lives down there. That’s wild.