
Exelon grabs attention for a simple reason: more and more families are searching for ways to help their loved ones manage memory loss. Unlike the hopeful stories you hear with new tech gadgets, this is deeply personal. When someone you care about starts forgetting names, repeating questions, or gets confused in their own home, it stings. Suddenly, a word like 'Exelon' can become as important as 'hope.' So what exactly makes this medication stand out? It’s not magic, but it can offer noticeable help if used right, and knowing more could help you make better choices.
What Is Exelon and How Does It Work?
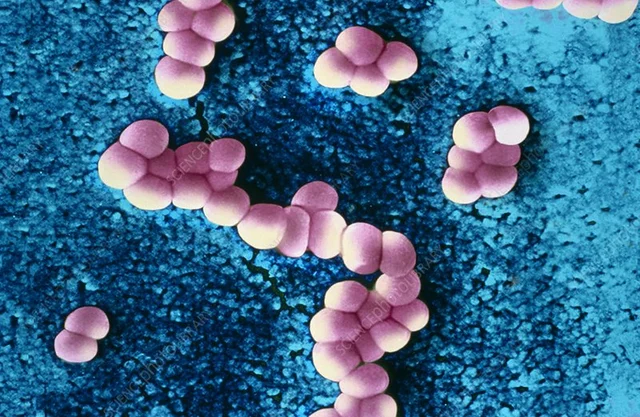
Exelon isn’t just a brand name you see on TV commercials featuring smiling grandpas and grandmas. It’s the trade name for rivastigmine, a medicine used to treat types of dementia like Alzheimer's disease and Parkinson’s disease dementia. Rivastigmine belongs to a family of drugs called cholinesterase inhibitors. Here’s the science in plain English: it works by boosting levels of a chemical in the brain called acetylcholine, which helps nerve cells talk to each other. In people with dementia, this chemical breaks down faster—the result is fuzzy memory, mixed-up thinking, and trouble with daily activities.
Doctors prescribe Exelon in two forms: a capsule (taken by mouth) and a patch (stuck on the skin). Why both versions? Swallowing pills can be tricky for some, especially as dementia progresses. The patch offers a slow, steady dose, and it sidesteps stomach issues for many people.
Rivastigmine has a bit of a special place among similar drugs because it’s approved for both Alzheimer’s and Parkinson’s dementia in the United States. Donepezil and galantamine—other cholinesterase inhibitors—are mostly just for Alzheimer’s. In other words, Exelon fills a gap when patients show signs of both memory and movement trouble.
But here’s what’s most important: Exelon isn’t a cure. It won’t stop dementia or reverse damage. What it can do is slow down some symptoms, especially in the earlier stages, so people can hold onto their daily routines and independence a bit longer. Research shows a modest improvement in memory and thinking for about 1 in 3 users. It’s not dramatic, but for families clinging to every day that feels 'normal,' it matters.
So, what does the science actually say? In a study cited by the American Journal of Psychiatry, patients on Exelon showed slower progression of memory problems compared to those on placebo over 24 weeks. Here’s a breakdown that helps put numbers to the claims:
| Study Duration | % with Improved Symptoms | % with No Change | % with Side Effects |
|---|---|---|---|
| 24 weeks | 32% | 55% | About 20% |
These numbers highlight two things: there’s hope for symptom management, but side effects aren’t rare. That’s why it’s crucial to weigh risks against benefits, and keep doctors in the loop.
Who Should Consider Exelon and How Is It Used?
Chances are, if you’re reading about Exelon, you’re either facing early signs of Alzheimer’s or Parkinson’s dementia, or you care for someone who is. Rivastigmine is FDA-approved for mild to moderate stages. Basically, it’s for people who are still able to dress, use the bathroom, and hold conversations, but are clearly struggling with memory and day-to-day tasks.
Here’s who doctors see as the 'right fit' for Exelon:
- Adults diagnosed with mild or moderate Alzheimer’s disease
- Those with Parkinson’s disease and related memory problems
- People who have tried other similar medicines, like donepezil, without much luck
Exelon comes in both capsules (usually taken twice a day with food) and skin patches (changed daily). The patch can be appealing because it keeps drug levels more stable and skips the need for remembering a pill schedule—something that isn’t always easy for someone with memory loss.
Starting Exelon isn’t one-size-fits-all. Doctors usually begin with a low dose to see how the body reacts. Over a few weeks, they may bump it up if needed, but only when side effects aren’t a problem. This slow ramp-up helps avoid tummy troubles and confusion, the most common initial complaints.
If you’re switching from pills to patches or vice versa (maybe because swallowing is tough), never make the change without checking first with a health professional. Patch users should pick a new spot on clean, dry skin each day—often the upper back, chest, or upper arm. If the skin gets red or itchy, try a different spot. Don’t slap a patch on the same location two days in a row.
Here’s a golden tip: keep a medication diary with daily notes about mood, confusion, and appetite. Over time, this helps you and your doctor spot improvements or side effects and make smarter choices about doses or switching medications.

Benefits and Limitations—What Can You Realistically Expect?
If you’re hoping Exelon is going to be a game-changer, it helps to know what’s realistic. Most people see small—sometimes hard-to-notice—improvements. Things like fewer memory lapses, better attention, and a little more confidence in daily routines. Don’t expect someone to suddenly recall childhood memories or become a social butterfly overnight.
Here’s what some users and families have shared:
- Getting dressed becomes less of a battle.
- Wandering or getting lost in familiar places happens less.
- Conversations feel less repetitive or stuck.
But there’s a flip side. About 1 in 5 people don’t see much difference at all. A small number even get worse—usually due to side effects. You’ll also want to keep your eyes open for the frustrations of the day-to-day: even with Exelon, dementia keeps creeping forward, so extra support at home is usually still needed. It’s best for families to think of this drug as a tool, not a solution.
Can Exelon stop someone from needing a nursing home? The studies are mixed, but sometimes it buys a few extra months at home. For caregivers, that can mean another summer together or simply delaying the tough conversations about long-term care.
If you notice someone getting more withdrawn, stubborn, or restless, make a note—these can be signs the benefits of Exelon are fading or that the disease is advancing. Experts suggest re-evaluating treatment every six months. That doesn’t mean quitting at the first setback, but it helps set realistic goals and avoid pointless costs or risk.
Side Effects and How to Handle Them
No drug is side-effect free, and Exelon is no different. In fact, stomach upset is the most common problem. Nausea, vomiting, and diarrhea show up in about 15-20% of users—but there are simple strategies that can help.
Take the capsule with a meal or snack to calm the stomach, or switch to the patch if pills are too rough. Itchy skin? Use the patch on different body parts each day—avoid hairy, oily, or broken skin, and hold off on hot showers or exercise right after putting on the patch, since sweat makes irritation worse.
Sometimes, the side effects are sneakier—weight loss, dizziness, trouble sleeping, or muscle weakness. More rarely, someone might faint or have a slow heartbeat, especially if they already take heart meds. Keep track of other drugs, and tell the prescribing doctor about every supplement and prescription, even eye drops. The risk of bad reactions goes way up the more meds you take.
Here’s a side-effect 'troubleshooting' table that comes from real clinic checklists:
| Problem | Common Cause | What Helps |
|---|---|---|
| Nausea/Vomiting | Starting dose too high | Take with food, lower dose, switch to patch |
| Skin rash | Using same patch spot | Rotate locations, moisturize skin |
| Dizziness | Low blood pressure, slow heart rate | Sit up slowly, check blood pressure, review meds |
| Confusion, agitation | Drug interactions, infection | Doctor review, check for other illnesses |
If you or a loved one seems suddenly out of sorts, don’t play guessing games. Call the doctor. Quick adjustments, or switching from capsule to patch, can make a world of difference.

Everyday Tips for Getting the Most from Exelon
Living with dementia isn’t about just picking the right pill—it’s about building routines and support. Exelon works best when paired with a steady schedule, regular meals, and simple reminders. Here are some survival strategies people swear by:
- Use a weekly pill organizer, or set smartphone alarms for dose times. Even caregivers can forget in the daily rush.
- For patches, write 'PATCH' on the bathroom mirror, or leave a sticky note on the fridge as a visual nudge.
- If swallowing is tough, ask about the patch—no more struggling with water, and fewer upset stomachs.
- Cut out heavy caffeine and late-night snacks, since Exelon sometimes causes nightmares or vivid dreams.
- Log changes, both good and bad, in a notebook or app to show your doctor clear patterns over time.
- Enroll in a support group if you’re a caregiver—navigating dementia alone is exhausting, and sharing tips with others can help.
Keeping up with hydration and nutrition matters more when taking Exelon. Dehydration, even mild, makes side effects worse. Watch weight and appetite, especially in folks with small frames who might shed pounds easily.
An underrated trick? Schedule daily activities at the same time each day. People with dementia do better with routines—so popping the pill or patch with breakfast and keeping events in the same order keeps everyone sane.
Want to stretch the benefits? Pair Exelon with gentle brain games, music, and walks around the neighborhood. These extras don’t replace meds, but they seem to boost quality of life, spark memories, and lower agitation for lots of folks.
And don’t forget: the most important part isn’t the medication; it’s patience and kindness, both for yourself and the person you’re helping. These days, all the little things matter—from a favorite song to a shared laugh—no matter what the calendar or memory says.
11 Comments
Jessica Forsen
July 19, 2025 AT 11:45 AM
Oh great, another wonder drug allegedly helping dementia but comes with side effects that seem fun, right? Sarcasm aside, I think it’s really important we temper expectations. I mean, sure, rivastigmine offers some improvement in cognitive skills, but it’s not like you’re turning your grandma into a super-genius or anything.
On the plus side, having something that can help slow decline is something at least. But let's be honest, it’s a bit like putting a Band-Aid on an enormous problem that needs serious care and understanding beyond just medication. The article does a decent job outlining practical advice, but I wish it didn’t gloss over how tough many patients find the side effects.
Also, I’d love more real statistics on long-term outcomes. Anyone have data on that?
Deepak Bhatia
July 20, 2025 AT 15:33 PM
I actually found this really helpful. My uncle started on Exelon last year, and the changes have been noticeable, even if small. It’s not a cure, but it helps with memory and daily tasks, at least for a while. What surprises me is how important the caregiver's role is alongside this medicine.
Many times, it’s about patience and understanding more than just the drug itself. I appreciate the practical tips here because doctors sometimes rush through explanations. Knowing what side effects to expect helped us prepare. It’s reassuring to see information that’s straightforward and clear.
Is anyone else here supporting a family member on this medicine?
Samantha Gavrin
July 21, 2025 AT 19:21 PM
You all are missing the bigger picture here. Have you considered what's really in these pharmaceuticals? I mean, sure, they say rivastigmine helps with dementia symptoms, but what about the hidden effects they don’t tell us? There's been some chatter about how drugs like these could be part of a larger scheme, influencing brain chemistry in ways we don’t fully understand or consent to.
I’m not saying don’t use it if it helps, but keep your eyes wide open. Medical industries have massive interests in keeping us dependent. Also, did anyone check if the drug has ingredients linked to other neurological issues down the line?
Just saying, be cautious and always demand transparent info from your doctors.
NIck Brown
July 22, 2025 AT 23:10 PM
While I appreciate the concerns here, I have to say that from my perspective, far too many people jump to cynicism without the proper understanding of neuropharmacology. Rivastigmine is an acetylcholinesterase inhibitor that specifically enhances cholinergic neurotransmission, which is crucial in dementia-related cognitive decline. Its efficacy, although not a cure, is well-documented in the literature.
Yes, side effects occur — mostly cholinergic side effects like gastrointestinal upset — but these are manageable with proper titration and monitoring. It's important not to demonize valuable treatments based on conspiracy theories or fears not grounded in evidence.
I'd encourage anyone with questions about mechanisms or safety profiles to consult the pharmacodynamics and pharmacokinetics data available.
Andy McCullough
July 24, 2025 AT 02:58 AM
Adding to the point about mechanisms, rivastigmine’s dual inhibition of acetylcholinesterase and butyrylcholinesterase is quite interesting. This dual action enhances cholinergic transmission in a broader range of brain regions compared to other agents. This can translate to more comprehensive symptom management in dementia patients, especially in Alzheimer's disease where cholinergic deficits are pronounced.
However, clinicians and caregivers should pay close attention to titration schedules because abrupt dose increases often lead to higher incidences of adverse events. Also, individual pharmacogenomic variations might influence both efficacy and tolerability, which is an emerging field worth considering.
Does anyone have experiences with dose adjustments or genetic testing related to this treatment?
Zackery Brinkley
July 25, 2025 AT 06:46 AM
Thanks for sharing all these perspectives. From my experience supporting a family friend in the UK with dementia, I'd say the key thing is balancing medication benefits and the overall care environment. Medication like Exelon can aid memory and cognitive function, but the social and emotional support really make a huge difference in quality of life.
It’s important not to rely solely on drugs but to combine them with care activities, exercise, and reassurance. Sometimes the medicine can feel like just a small piece of a very complex puzzle.
It's good to see posts like this helping to break down information for everyday people. That really empowers carers and families.
Luke Dillon
July 26, 2025 AT 10:35 AM
This article hits most of the right points from what I’ve seen working with dementia patients. The side effects can discourage some people from continuing, especially early on, but with patience the body often adjusts. What’s great is how rivastigmine can provide extended periods of mental clarity for some people, which is invaluable in maintaining independence.
Also, something to mention is checking for drug interactions if the patient is on other medications. That’s a big factor that isn’t emphasized enough. Always consult healthcare providers about the full medication profile.
Would be interested to hear if anyone noticed differences between the patch form and capsules in terms of side effects and efficacy.
Elle Batchelor Peapell
July 27, 2025 AT 14:23 PM
Thinking beyond what the medication does, I wonder about the philosophical aspect of treating dementia with drugs like rivastigmine. I mean, isn't it a delicate balance between prolonging cognitive function and respecting the natural progression of the disease?
When we intervene medically to alter brain chemistry, it raises questions about identity and selfhood. How much of someone’s personality or essence remains when these drugs change the way their brain works? The nuances of benefit versus alteration make this a fascinating subject.
This isn’t to undermine the importance of the drug’s benefits, but rather to highlight that dementia care is as much about what medicine can’t fix as what it can.
Jeremy Wessel
July 28, 2025 AT 18:11 PM
Concise and practical response here: rivastigmine remains one of the frontline agents in mild to moderate dementia management, mainly due to its reversible and competitive ChE inhibition, which boosts central cholinergic activity implicated in cognitive processes.
Its action on butyrylcholinesterase, alongside acetylcholinesterase, provides a pharmacological advantage over other drugs in its class. Clinicians must be attentive to titration, as abrupt escalation risks cholinergic crisis symptoms.
Also, monitoring for adverse cardiac and gastrointestinal effects should be standard. It is imperative patients/caregivers be briefed on expected side effects and management strategies.
Laura Barney
July 29, 2025 AT 22:00 PM
Thanks for compiling this info! I feel like compassionate caregiving is often overshadowed by just focusing on meds. Sure, rivastigmine offers some cognitive stability, but the emotional and social support are just as important for those with dementia. The article's practical tips about side effect monitoring and dosage remind us that every patient reacts differently.
Also wanted to add that openness to adjusting treatment plans is key. Listening closely to the person’s experience can help tailor medication and create more positive outcomes. The colorful complexity of dementia calls for a flexible, creative, and patient approach in medicine and care.





Susan Hayes
July 18, 2025 AT 07:58 AM
Honestly, if you're considering Exelon for someone with dementia, you better know what you're getting into. Rivastigmine isn't some miracle drug; it has benefits, sure, but the side effects can be brutal. People often underestimate how tough it can be to tolerate this medication. Nausea, dizziness, and even more severe reactions aren't uncommon, so don't just jump on the bandwagon blindly.
It’s supposed to improve cognitive function, but how much does it really help? From what I’ve seen, the effects are marginal at best and usually short-lived. If you expect it to reverse dementia symptoms, think again. Still, for some, the slight improvement makes a difference in day-to-day quality of life. Just prepare for the ride, because it can be pretty rough.
And don’t forget, managing dosage properly is critical. Encouraging your loved one to communicate any side effects is vital; otherwise, you might end up with more harm than good.