
Getting the right dose of medicine for a child isn’t just tricky-it’s life-or-death. A child’s weight, age, and even developmental stage change how much medicine they need. One wrong decimal point, one mix-up between pounds and kilograms, and you could be giving a 300% overdose. That’s not hypothetical. In 2024, a 22-month-old in Ohio received a dangerous overdose of ibuprofen because a parent entered weight in pounds instead of kilograms in a free app that didn’t warn them. This isn’t rare. Medication errors in kids happen up to three times more often than in adults, according to the Institute for Safe Medication Practices.
Why Pediatric Dosing Is So Different
Adults usually get fixed doses: one pill, one tablet, one teaspoon. Kids don’t. Their doses are calculated by weight-usually in kilograms. A 5-kilogram baby needs a tiny fraction of what a 25-kilogram toddler needs. That means every time you give medicine, you’re doing math. And math under stress? That’s where mistakes happen. Think about it: it’s 2 a.m., your child has a fever, you’re half-asleep, and you’re trying to figure out if 2.5 mL of acetaminophen is right for a 12-pound baby. You grab a paper chart from the hospital, squint at tiny print, and hope you didn’t misread the column. Or worse-you guess. That’s where apps and dosing charts come in. They don’t replace judgment, but they cut out the guesswork. Studies show digital tools can reduce dosing errors by 43% and cut calculation time by 67% compared to paper charts.Tools for Clinicians: Speed, Accuracy, and Emergency Readiness
In hospitals and ERs, time is everything. That’s why tools like Pedi STAT is a mobile application developed by Connecticut Children's Medical Center to provide rapid, accurate pediatric dosing calculations in emergency situations, featuring automatic weight conversion and 200+ medication protocols were built. It’s not fancy-it’s fast. You tap in a child’s weight in kilograms (or pounds, if you’re trained to convert), and within three seconds, it gives you the exact dose for epinephrine, albuterol, or antibiotics. No scrolling. No math. It’s used in over 89% of U.S. children’s hospitals. Version 4.2.1, updated in May 2023, works on iOS 14+ and Android 8+. It’s 87 MB, lightweight, and designed for chaos. A 2022 study in Pediatric Emergency Care found that manual calculations took 18.7 seconds and had a 12.3% error rate. Pedi STAT? Three seconds. Less than 1% error. Then there’s Epocrates is a clinical decision support app with a database of over 4,500 pediatric medications, drug interaction checks, and dosing guidelines, widely used by healthcare professionals since 1998. It’s like the Swiss Army knife for doctors. It doesn’t just dose-it warns you if the medicine conflicts with another drug the child is on. It’s got 35,000+ interaction alerts. But it’s not built for speed in emergencies. It’s better for routine rounds. And for reference? The Harriet Lane Handbook is a trusted clinical reference for pediatric dosing, containing guidelines for over 600 medications, used by professionals in hospitals and academic centers is the gold standard. But it’s dense. It’s written for med students and residents. You need a $70 annual subscription. It’s not for parents. It’s for experts.Tools for Parents: Simplicity, Reminders, and Peace of Mind
At home, you don’t need a medical dictionary. You need a calendar. A reminder. A way to know if you already gave the medicine-or if you gave too much. That’s where My Child's Meds is a parent-focused app developed with input from the Royal College of Paediatrics and Child Health, offering medication scheduling, double-dose prevention, and visual tracking for home use without subscription fees comes in. It’s free. It’s simple. You add your child’s name, weight, and medications. It sets up a daily schedule. When it’s time, it pings you. If you try to log a dose too soon after the last one, it blocks you. It even uses color-coded icons-green for given, red for missed-so you can glance at your phone and know at a glance. Parents using it report a 38% drop in dosing errors. One mom in New Zealand wrote: “This app saved us when my toddler’s fever schedule got messed up during night feedings. I almost gave him the same dose twice. The app stopped me.” Another popular option is NP Peds MD is a pediatric dosing reference app developed by Northpoint Pediatrics, offering approved dosage tables by weight for common OTC medications, designed for caregiver use. It doesn’t track schedules. It gives you clear charts: “If your child weighs 10-14 kg, give 5 mL of ibuprofen.” No math. Just match the weight to the number. A 2024 Consumer Reports study found parents using this app got the dose right 78% of the time. With paper charts? Only 52%.
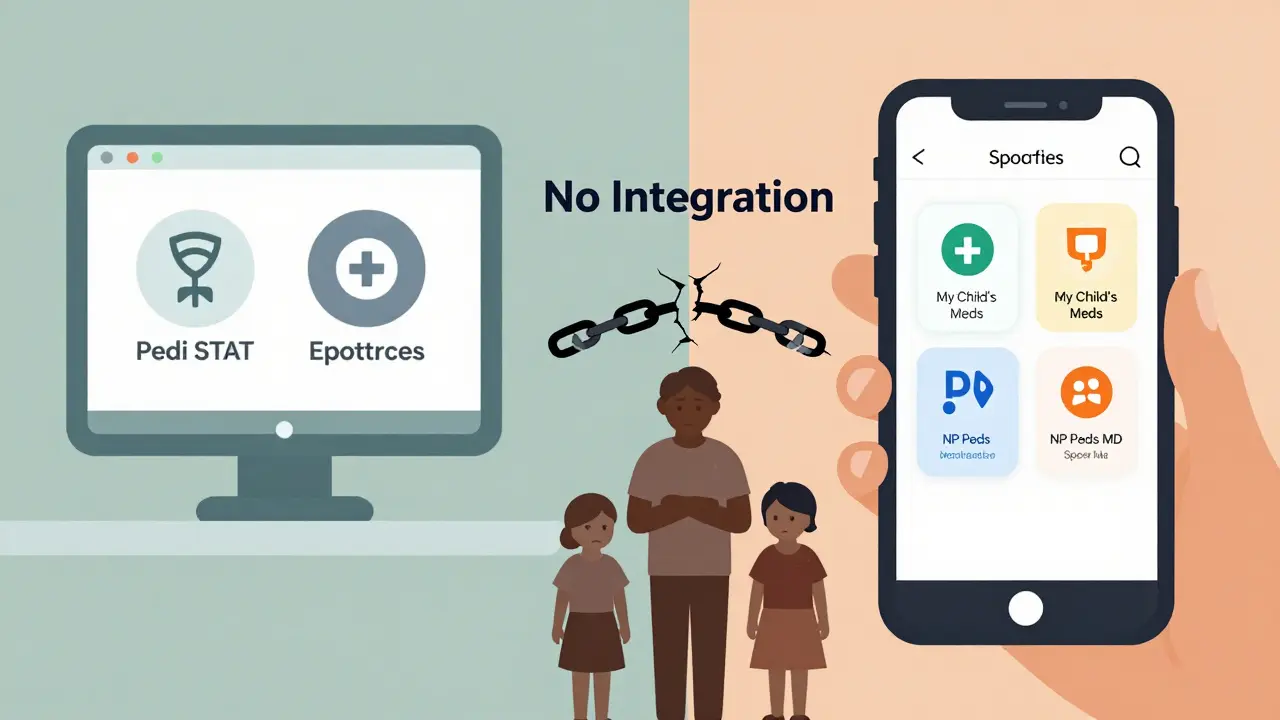
The Big Problem: No One Talks to Each Other
Here’s the catch. Your hospital uses Pedi STAT. Your doctor uses Epocrates. Your pharmacist uses a different system. And your phone has My Child’s Meds. None of them talk to each other. That’s why 87% of medication errors in kids happen during care transitions-when a child goes from hospital to home. The discharge nurse gives you a paper list. You try to type it into your app. You miss a dose. You double up. You get confused. A 2023 American Academy of Pediatrics survey found that 68% of parents struggle to transfer medication info from hospital instructions to their home app. That’s not your fault. It’s the system’s. Even worse: some apps claim to help but are just digital notebooks. Child Medical History is a consumer app that stores medication logs and health records but does not calculate doses or provide clinical guidance costs $3.99. It lets you write down what you gave your kid. But it doesn’t tell you if it’s the right amount. That’s like buying a notebook for your car’s oil change and thinking it’ll tell you how much to put in.How to Use These Tools Safely
Apps aren’t magic. They’re tools. And tools can be dangerous if you don’t know how to use them. Here’s how to stay safe:- Always check the unit. Kilograms or pounds? Most apps let you pick. But if you pick pounds and your child’s weight is in kilograms, you’ll overdose. Always double-check the unit before you hit calculate.
- Verify with a second source. If the app says 4 mL, look at the bottle. Look at the chart from the hospital. Cross-check.
- Never trust free apps from unknown developers. Stick to apps developed by hospitals, pediatric associations, or pharmacies. Avoid random apps with no clear publisher.
- Keep a paper backup. Phones die. Apps crash. Power goes out. Always have a printed dosing chart from your doctor or pharmacist.
- Do a weekly reconciliation. Every Sunday, compare your app’s log with your pharmacy’s refill record. If the numbers don’t match, call your doctor.
What’s Coming Next
The future is getting smarter. Pedi STAT is testing AI that predicts when a parent is likely to make a mistake-like giving a dose too early-and sends a warning before they tap “administer.” Boston Children’s Hospital is trialing smart pill dispensers that only unlock the right dose at the right time. And HIMSS is working on a new data standard to let hospital apps talk to home apps-finally. By 2027, nearly all pediatric doses in hospitals will be verified digitally. That’s good. But for that to work at home, parents need better tools, better training, and better connections between the hospital and the kitchen table.What to Do Today
If you’re a parent:- Download My Child’s Meds (iOS only, free).
- Enter your child’s weight in kilograms (not pounds).
- Add every medication-even vitamins and OTC stuff.
- Turn on reminders and double-dose alerts.
- Print a backup chart from your pharmacist.
- Use Pedi STAT in emergencies. Train your team.
- Recommend My Child’s Meds or NP Peds MD to parents.
- Never assume the family understands the dose. Show them. Let them repeat it back.
When to Call for Help
If you’re ever unsure:- Call your pharmacist. They’re trained for this.
- Call your pediatrician. Don’t wait.
- If your child shows signs of overdose-drowsiness, vomiting, irregular breathing-call emergency services immediately.
Can I trust free pediatric dosing apps?
Only if they’re made by trusted organizations like hospitals, pediatric associations, or pharmacies. Avoid random apps with no clear developer. Apps like My Child’s Meds and NP Peds MD are developed with clinical input and are free. Many free apps from unknown publishers don’t calculate doses correctly-or at all. They’re just digital notebooks.
Should I use an app instead of a paper dosing chart?
Use both. Apps are faster and reduce errors, but phones die, apps crash, and power can go out. Always keep a printed copy from your doctor or pharmacist. Use the app for reminders and tracking, but verify the dose with the paper chart before giving medicine.
What’s the difference between Pedi STAT and My Child’s Meds?
Pedi STAT is for doctors and nurses in emergencies. It calculates doses for 200+ medications in seconds. My Child’s Meds is for parents at home. It tracks schedules, sends reminders, and prevents double dosing. They serve different roles. One saves lives in the ER. The other prevents mistakes at 3 a.m.
Why do I need to enter my child’s weight in kilograms?
All pediatric dosing guidelines are based on kilograms (kg), not pounds. If you enter pounds but the app expects kilograms, it will calculate a dose that’s way too high. For example, a 22-pound child is about 10 kg. If you enter 22 as kilograms, the app thinks they weigh 48 pounds-and gives them almost double the right dose. Always double-check the unit.
Do these apps work with electronic health records?
Professional apps like Pedi STAT and Epocrates can connect to hospital systems like Epic or Cerner-but only if the hospital sets it up. Parent apps like My Child’s Meds cannot connect to hospital records due to privacy laws. That’s why transferring info between hospital and home is still a major problem. Always bring your app log to appointments.
Is there an app for multiple children?
Yes. My Child’s Meds lets you create separate profiles for each child. You can switch between them easily. This is essential if you have more than one child on medication. Don’t mix up their schedules. Each profile keeps their weights, meds, and reminders separate.
What if my child’s weight changes?
Update the weight in your app every time your child gains or loses a significant amount-usually every 3-6 months. Dosing is based on weight, so even a 2-kilogram change can affect the dose. If you’re unsure, call your pediatrician before giving the next dose.
11 Comments
Sarah Williams
December 20, 2025 AT 16:33 PM
This post should be mandatory reading for every new parent. Seriously. I didn’t know how dangerous simple dosing mistakes could be until my kid had a fever scare. Apps aren’t perfect, but they’re way better than guessing at 3 a.m.
Michael Ochieng
December 22, 2025 AT 14:07 PM
I work in a pediatric ER and we use Pedi STAT on every shift. It’s not glamorous, but it’s the reason we haven’t had a dosing error in over two years. Train your nurses. Use it. Trust it. It’s not magic-it’s math you don’t have to do.
Also, if you’re a parent and you’re using some random app from the App Store with no logo from a hospital, delete it. I’ve seen apps that convert kg to lb backwards. That’s not a glitch-that’s a hazard.
Theo Newbold
December 24, 2025 AT 12:55 PM
Let’s be real-this whole app movement is just another way for Big Pharma to shift liability onto parents. Hospitals use their own systems. Doctors use Epocrates. But you? You’re supposed to trust some free app that doesn’t even have a privacy policy? The fact that they’re pushing this on families while the system stays disconnected is criminal.
And don’t get me started on ‘My Child’s Meds.’ It’s literally just a digital notepad with a ping. No clinical validation. No FDA oversight. Just a pretty interface and a false sense of security.
Dan Adkins
December 25, 2025 AT 03:14 AM
It is imperative to underscore the critical importance of standardized weight input protocols in pediatric pharmacology. The utilization of kilograms as the sole metric for dosage calculation is not merely a convention-it is a non-negotiable standard grounded in international clinical guidelines, including those promulgated by the World Health Organization and the American Academy of Pediatrics. The casual conversion of pounds to kilograms by laypersons, particularly under conditions of acute stress, constitutes a systemic vulnerability that must be addressed through institutional mandates, not consumer applications.
Furthermore, the proliferation of non-clinical apps such as My Child’s Meds, while well-intentioned, introduces a dangerous layer of epistemic dissonance. These tools lack the ontological rigor required for medical decision-making and thereby undermine the professional authority of the clinician-patient relationship. One does not entrust the calibration of a surgical instrument to a smartphone application; one should not entrust the administration of life-sustaining medication to one either.
Adrian Thompson
December 26, 2025 AT 16:13 PM
Of course the government wants you using apps. So they can track your kid’s meds, build a profile, and eventually force you to use their ‘approved’ dosing schedule. Next thing you know, they’ll block the app if your kid’s weight is ‘too high’ or if you’re not ‘compliant.’ They’ve been doing this with vaccines for years. Don’t fall for it.
And Pedi STAT? That’s just a front for the CDC’s national pediatric monitoring program. Why do you think it’s in 89% of hospitals? Coincidence? I don’t think so.
Erika Putri Aldana
December 28, 2025 AT 00:41 AM
Why do we even need apps? Isn’t it just… parenting? I mean, come on. We used paper charts in the 80s and we didn’t have kids dying left and right. Maybe we just need to stop being lazy and actually pay attention?
Also, I think the whole ‘kilograms vs pounds’ thing is a scam. Everyone knows a kid weighs 20 pounds. Why make it complicated? Just eyeball it. If they look like they need half a spoon, give half a spoon. Done.
Also, why is everyone so scared of overdosing? Kids are tough. They bounce back. We used to give them aspirin for fevers and no one died. Just saying.
Southern NH Pagan Pride
December 29, 2025 AT 19:31 PM
Did you know that the ‘free’ apps like My Child’s Meds are secretly synced to the National Pediatric Surveillance Network? They’re not just tracking doses-they’re collecting biometric data to feed into the CDC’s predictive overdose AI. The ‘double-dose alert’? That’s not protection. That’s a trigger. When it blocks you, it’s because the algorithm decided your child is ‘high-risk’ and flagged your household.
And Pedi STAT? Developed by a hospital that got a $47 million grant from Pfizer in 2021. Coincidence? I don’t think so. They want you dependent on their system so they can control the narrative when the next ‘outbreak’ happens. Paper charts are the only safe option. Print them. Laminate them. Hide them in your sock drawer.
Also, why do all the apps only work on iOS? That’s not an accident. Apple is in bed with Big Pharma. Android users are being left behind on purpose. Wake up.
Peggy Adams
December 31, 2025 AT 00:38 AM
Ugh. Another ‘parenting hack’ post. Can we just admit that most of this stuff is overkill? I gave my kid Tylenol for a year with a paper chart and never messed up. I didn’t need an app to remind me. I just… remembered.
Also, why is everyone so scared of a little math? It’s not rocket science. 10 kg = 22 lbs. You multiply by 10. Done. If you can’t do that, maybe you shouldn’t be giving medicine at all.
And the ‘free app’ thing? I downloaded one last year. It asked for my kid’s birth certificate and my home address. Nope. Not happening. I’ll stick with the paper.
Jerry Peterson
December 31, 2025 AT 22:30 PM
Just want to say-this post saved my sanity. I used to panic every time my daughter had a fever. Then I found My Child’s Meds. I print the chart every time we get a new prescription. I show the pharmacist. I double-check the bottle. I still get nervous. But now I’m nervous with a plan.
Also, to the guy who said ‘kids are tough’-you’re right. But they’re also small. And small things break easier. I’d rather be overcautious than sorry.
Michael Ochieng
January 2, 2026 AT 11:21 AM
Hey @JerryPeterson-your comment about printing charts? That’s exactly what we tell families in the ER. I’ve seen parents bring in their phone with the app open… and the battery’s dead. Or the app crashed. Or they forgot the password. That’s when the paper saves them.
Also, thanks for saying ‘I’m nervous with a plan.’ That’s the whole point. It’s not about being perfect. It’s about having layers. App + paper + pharmacist check. That’s how you win.




Meina Taiwo
December 20, 2025 AT 14:50 PM
Just use My Child’s Meds. Free, simple, no ads. Saved my life when my twins were on different meds. No math, just tap and go.