
Every winter, millions of people reach for nasal decongestants to clear their sinuses. But if you’re taking medication for high blood pressure, that little bottle of Sudafed could be hiding a serious risk. You might not realize it, but the same ingredient that shrinks swollen nasal passages can also spike your blood pressure - sometimes dangerously so. This isn’t just a warning on a label. It’s a real, documented danger that sends people to the ER every year.
How Decongestants Work (and Why They’re Risky)
Nasal decongestants like pseudoephedrine and phenylephrine work by tightening blood vessels. That’s why your nose clears up - less swelling, less mucus. But here’s the catch: those blood vessels aren’t just in your nose. They’re everywhere - including in your heart, brain, and kidneys. When these drugs tighten them systemically, your blood pressure rises. It’s not a small bump. Studies show pseudoephedrine can raise systolic blood pressure by 2 to 5 mmHg on average. For someone with uncontrolled hypertension, that’s enough to trigger a headache, chest pain, or even a stroke.
And it’s not just oral pills. Topical sprays like Afrin (oxymetazoline) aren’t safe either. Many people think because it’s applied in the nose, it stays there. But research from the University of Michigan Health System shows up to 30% of the drug can enter your bloodstream. That’s enough to interfere with your blood pressure meds. Even one or two days of use can be risky if you’re already on medication.
Which Decongestants Are the Most Dangerous?
Not all decongestants are created equal. The big three to watch out for are:
- Pseudoephedrine - Found in Sudafed, Claritin-D, Zyrtec-D, and many cold and flu combos. This is the strongest and most studied. It’s behind the pharmacy counter in the U.S. for a reason.
- Phenylephrine - Now the most common OTC decongestant after pseudoephedrine was restricted. But don’t be fooled. A 2024 study in the Journal of Clinical Hypertension found it still raises blood pressure, especially in higher doses or with repeated use.
- Ephedrine - Rare in the U.S. now, but still found in some herbal supplements and older products. Extremely dangerous for heart patients.
And here’s the sneaky part: you won’t always see them listed as “decongestant.” Check the active ingredients on any cold, flu, or allergy medicine. If you see any of those three names, put it back. Even if the box says “sinus relief” or “congestion formula,” it’s likely hiding a decongestant.
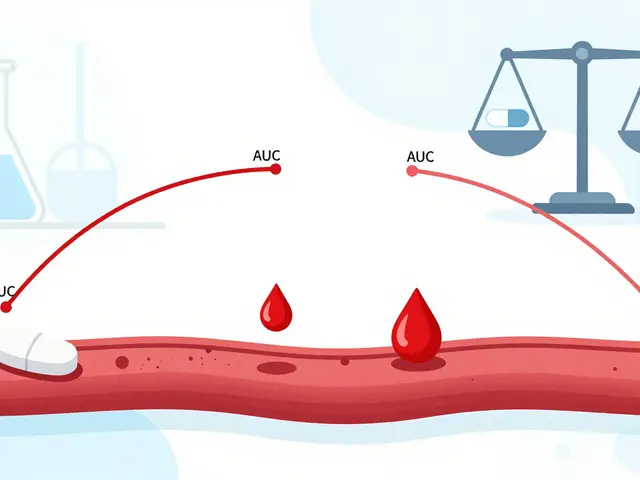
How They Interfere With Your Blood Pressure Meds
It’s not just about raising your numbers. Decongestants can make your blood pressure medications less effective - or even cause dangerous interactions.
For example:
- With beta-blockers like metoprolol, decongestants can cause your heart to race or beat irregularly.
- With calcium channel blockers like nifedipine or felodipine, the combined effect can lead to severe spikes in blood pressure.
- With MAO inhibitors (used for depression or Parkinson’s), decongestants can cause a life-threatening surge in blood pressure called a hypertensive crisis.
Even common painkillers like ibuprofen or naproxen can worsen the problem. They raise blood pressure too, and many cold formulas combine them with decongestants. You’re not just taking one risky drug - you’re stacking them.

What to Do Instead: Safer Ways to Clear Your Nose
You don’t need to suffer through congestion. There are safer, effective alternatives - and many work just as well without the risk.
- Nasal saline spray - Plain saltwater rinses or sprays (like NeilMed or store-brand saline) moisten your nasal passages and flush out mucus. No drugs. No side effects. Use it as often as you need.
- Steam inhalation - Take a hot shower, or lean over a bowl of hot water with a towel over your head. The steam loosens mucus and reduces swelling naturally.
- Antihistamines - If your congestion is from allergies (not a cold), drugs like loratadine (Claritin) or cetirizine (Zyrtec) can help. They don’t raise blood pressure. Just know they’re slower to work - they’re not instant relief like decongestants.
- Humidifiers - Keeping the air moist helps your nasal passages stay open. Especially useful at night.
Dr. Salman Al-Kindi at Houston Methodist Hospital says, “For most people with heart conditions, home remedies are enough.” You don’t need a chemical fix for a virus that will run its course in a week.
How to Read Labels Like a Pro
Most people don’t know what to look for. Here’s how to avoid the traps:
- Always check the “Active Ingredients” section - not the front of the box.
- Look for: pseudoephedrine, phenylephrine, oxymetazoline, ephedrine.
- Watch for “D” in product names - Claritin-D, Zyrtec-D, Allegra-D - that means “decongestant.”
- Even “allergy” or “sinus” formulas often contain decongestants. Don’t assume.
- Check for sodium content. Some cold medicines have over 200mg of sodium per dose - and salt raises blood pressure too.
When in doubt, leave it on the shelf. Better to be safe than sorry.

When You Absolutely Must Use a Decongestant
There are rare cases - like severe sinus infection or blocked Eustachian tubes - where a doctor might approve short-term decongestant use. If that’s you:
- Only use it if your doctor says yes - and get the exact dose.
- Use the lowest dose possible for the shortest time - no more than 3 days.
- Monitor your blood pressure twice a day while using it. If it rises more than 10 points, stop immediately.
- Never combine it with other stimulants like caffeine, nicotine, or weight-loss pills.
And remember: even if your blood pressure is “controlled,” that doesn’t mean it’s safe. The Cleveland Clinic says bluntly: “Don’t take nasal decongestants if you have unmanaged high blood pressure - even if you think yours is managed.”
Ask Your Pharmacist - Seriously
Pharmacists are your secret weapon. In the U.S., pseudoephedrine is kept behind the counter because it can be misused. But that also means you get a free consultation. Don’t just grab it and walk out. Say: “I’m on blood pressure medication. Is this safe?”
Studies show pharmacist-led counseling reduces inappropriate decongestant use by nearly half. That’s not just helpful - it’s life-saving.
What You Should Do Right Now
Here’s your action list:
- Check every cold, flu, and allergy medicine in your cabinet. Look for pseudoephedrine, phenylephrine, or oxymetazoline.
- Make a list of all your medications - prescription, OTC, supplements - and bring it to your next doctor’s visit.
- Replace your current decongestant with saline spray or steam therapy.
- Ask your pharmacist to review your meds during your next visit.
- Set a reminder to check your blood pressure more often during cold season.
High blood pressure is manageable. But it’s also fragile. A single over-the-counter pill can undo months of careful control. You’ve worked hard to keep your numbers in check. Don’t let a cold knock you back.
Can I use nasal saline spray if I have high blood pressure?
Yes, absolutely. Nasal saline sprays contain only salt and water. They don’t affect blood pressure, heart rate, or interact with any medications. They’re the safest option for clearing congestion if you have hypertension.
Is phenylephrine safer than pseudoephedrine for high blood pressure?
No. While pseudoephedrine has stronger effects, phenylephrine still raises blood pressure. A 2024 study found it causes measurable increases in systolic pressure, especially with repeated use. Neither is safe without a doctor’s approval.
Can I take decongestants if my blood pressure is under control?
Even if your blood pressure is controlled, decongestants can still cause dangerous spikes. The Cleveland Clinic and American Heart Association advise against them regardless of control status. Always consult your doctor first.
Do topical nasal sprays like Afrin affect blood pressure?
Yes. Though applied locally, oxymetazoline (the active ingredient in Afrin) enters the bloodstream. Studies show it can raise blood pressure, especially with prolonged use. Avoid it unless your doctor says it’s safe.
What should I do if I accidentally took a decongestant?
Stop taking it immediately. Check your blood pressure. If it’s more than 10 points higher than your usual reading, or if you feel dizzy, chest tightness, or a rapid heartbeat, call your doctor or go to urgent care. Don’t wait for symptoms to get worse.
Are there any decongestants approved for people with high blood pressure?
As of 2026, there are no OTC decongestants considered safe for people with high blood pressure without medical supervision. Some pharmaceutical companies are testing new non-vasoconstrictive alternatives, but none are available yet. Stick to saline, steam, and antihistamines.
15 Comments
Tru Vista
January 3, 2026 AT 10:24 AM
Phenylephrine is useless anyway. The FDA admitted it’s not effective. So why is it everywhere? Corporate greed. They replaced pseudoephedrine because it was hard to make meth with, not because it’s safer. You’re being sold a placebo that still kills you. Classic.
Joy F
January 5, 2026 AT 06:43 AM
It’s not just about blood pressure. It’s about the quiet betrayal of capitalism. We’re told to ‘take charge of our health’ while the system floods the shelves with slow-poison pills disguised as relief. That little blue bottle? It’s not medicine-it’s a Trojan horse for corporate profit. And we’re the ones who swallow it. Literally. We’re not sick. We’re exploited.
Lori Jackson
January 6, 2026 AT 10:19 AM
As someone who’s spent 12 years in clinical pharmacology, I must say: this post is *barely* scratching the surface. The real issue is polypharmacy cascades-decongestants don’t just interact with antihypertensives; they dysregulate the RAAS axis, amplify sympathetic tone via alpha-1 agonism, and suppress baroreflex sensitivity. Most patients don’t even know what ‘sympathetic tone’ means. They just want to breathe. But ignorance isn’t bliss-it’s a prelude to a hypertensive emergency. I’ve seen three strokes in six months from this exact combo. Stop being casual. This is a public health crisis.
veronica guillen giles
January 7, 2026 AT 07:52 AM
Wow. So we’re supposed to trust a post that says ‘ask your pharmacist’ but doesn’t mention that 60% of pharmacists in rural areas don’t have time to counsel you? 😒 Also, saline spray? Cute. I have a deviated septum and a 10-year-old with a runny nose. Steam? At 3am? With a screaming kid? Give me a break. This feels like a luxury wellness blog for people who don’t actually live in the real world.
Haley Parizo
January 7, 2026 AT 23:38 PM
There’s a deeper truth here: we’ve outsourced our bodies to corporations. We don’t trust our own healing capacity anymore. We reach for a pill because we’ve been taught that discomfort is a problem to be solved, not a signal to be listened to. Congestion isn’t the enemy. Our relationship with medicine is. The real cure? Slowing down. Breathing. Letting the body do what it’s designed to do. The spray? The steam? The silence? Those are the real remedies. The pills are just noise.
Michael Burgess
January 9, 2026 AT 06:03 AM
Just wanted to say thank you for this. I’m on lisinopril and had no idea Afrin was risky. I used it for 5 days last month and felt like my heart was trying to escape my chest. Now I keep saline spray by my bed. Also, steam with eucalyptus oil? Game changer. 🙌
Palesa Makuru
January 9, 2026 AT 14:03 PM
Oh honey, I’m so glad you mentioned the sodium content. I didn’t even think about that. I’ve been taking those ‘low-sodium’ cold meds thinking they were safe… until I read the label and saw 230mg per dose. That’s like eating a whole bag of pretzels. I’m done. I’m switching to nasal irrigation. My nose hates me, but my BP loves me now. 💅
Neela Sharma
January 10, 2026 AT 21:56 PM
My grandmother used to say: ‘If it burns your nose, it’s not healing you.’ She’d boil rosemary, inhale the steam, and rub mustard oil on her chest. No pills. No panic. Just breath. We forgot how to listen to our bodies. We replaced wisdom with labels. Let’s return to the old ways-not because they’re ‘natural,’ but because they’re gentle. The body remembers. It just needs space.
innocent massawe
January 12, 2026 AT 21:47 PM
Thank you for this. In Nigeria, people use decongestants like candy. No one checks labels. My uncle had a stroke last year because he took Sudafed for a cold. He didn’t even know he had high BP. This info could save lives here. Please share this more.
Vincent Sunio
January 13, 2026 AT 11:16 AM
While the sentiment is commendable, the post exhibits a concerning lack of nuance regarding phenylephrine’s pharmacokinetics. The 2024 study cited demonstrates only marginal elevation in systolic pressure under controlled conditions; real-world variability is substantial. Moreover, the assertion that ‘no OTC decongestants are safe’ is an overgeneralization that disregards individual pharmacogenomic profiles. One must consider CYP450 metabolism, renal clearance, and comorbidities-not just binary ‘safe/unsafe’ dichotomies. This is alarmist oversimplification masquerading as medical advice.
Ian Detrick
January 14, 2026 AT 01:19 AM
Look-I get it. You’re scared. I was too. But don’t let fear paralyze you. Use saline. Use steam. Use a humidifier. And if you’re really struggling? Talk to your doctor. Don’t just panic and avoid everything. There’s a middle ground. You don’t have to suffer. You just have to be smart. You’ve got this.
Shruti Badhwar
January 14, 2026 AT 10:10 AM
While the article presents a compelling case, it fails to address the socioeconomic barriers to implementing these alternatives. Saline sprays are not covered by insurance in many U.S. states. Steam requires time, heat, and a private space-luxuries not available to shift workers or those in overcrowded housing. The advice, while medically sound, is classist in its assumptions. We must advocate for systemic change, not just individual behavioral fixes.
Angela Fisher
January 15, 2026 AT 20:32 PM
EVERYTHING IS A CONSPIRACY. I’ve been tracking this for years. The FDA allows phenylephrine because it’s funded by Big Pharma. The ‘studies’? Fabricated. The ‘pharmacist advice’? Paid actors. They want you to think you’re safe with saline-until they patent the next ‘miracle’ nasal gel that’s just decongestant #4 in disguise. They’re watching you right now. Your smart fridge knows you bought saline spray. They’re testing your BP remotely. Don’t trust anything. Not even this post. 😈
Ian Ring
January 16, 2026 AT 16:25 PM
Well, this was... a lot. But honestly? Needed it. I’ve been on amlodipine for 8 years. Never thought about decongestants. Just grabbed whatever was on sale. Now I’ve got a sticky note on my medicine cabinet: ‘NO D. NO OX. NO PHENYL.’ And I’m buying saline. Thanks. 🙏




Wren Hamley
January 2, 2026 AT 18:23 PM
Okay but let’s be real-how many of us have grabbed a cold med without checking the label? I did it last winter. Thought ‘sinus relief’ meant ‘just stuff to unclog my nose.’ Turns out I was holding a chemical firecracker. My BP spiked to 170/100 after two doses. Scared the hell out of me. Now I read every tiny font like it’s a legal contract. Not fun, but life-saving.