
Living with fibromyalgia isn’t about finding a cure. It’s about learning how to live well despite the pain. There’s no magic pill, no quick fix. But thousands of people - mostly women - are finding ways to reduce their symptoms, get back some control, and rebuild their days around what they can do, not what they can’t. If you’re dealing with constant muscle aches, crushing fatigue, brain fog, or sleep that never feels restful, you’re not alone. And there are real, evidence-backed ways to make things better.
What Fibromyalgia Actually Feels Like
Fibromyalgia isn’t just "feeling tired" or having sore muscles after a long day. It’s a neurological condition where your nervous system gets stuck on high alert. Pain signals amplify. Even light touches can hurt. You might wake up exhausted even after eight hours of sleep. Concentrating feels like wading through mud. Flare-ups can hit out of nowhere - one day you’re fine, the next you can barely get out of bed.
The American College of Rheumatology recognized fibromyalgia as a real condition back in 1990. Today, about 4 million Americans live with it, and women make up 75 to 90% of cases. There’s no blood test, no X-ray that confirms it. Diagnosis comes from ruling out other conditions and matching symptoms to established criteria. That doesn’t make it less real. It just means managing it takes a different approach.
Pain Control: Medications That Actually Help
Three drugs are FDA-approved specifically for fibromyalgia: duloxetine (Cymbalta), milnacipran (Savella), and pregabalin (Lyrica). These aren’t painkillers like ibuprofen. They work on how your brain processes pain signals.
Studies show these medications can reduce pain by about 30-40% compared to a placebo. That might sound modest, but for someone stuck at an 8 out of 10 on the pain scale, dropping to a 5 or 6 can mean the difference between staying in bed and making breakfast. Pregabalin can cause dizziness or weight gain - side effects that make some people quit. Duloxetine often causes nausea, especially at first.
Doctors also use other drugs off-label, like gabapentin, amitriptyline, or antidepressants like sertraline. But here’s the catch: only about 25% of patients get half their pain relief from medication alone. That’s why most experts say meds should be just one part of the plan.
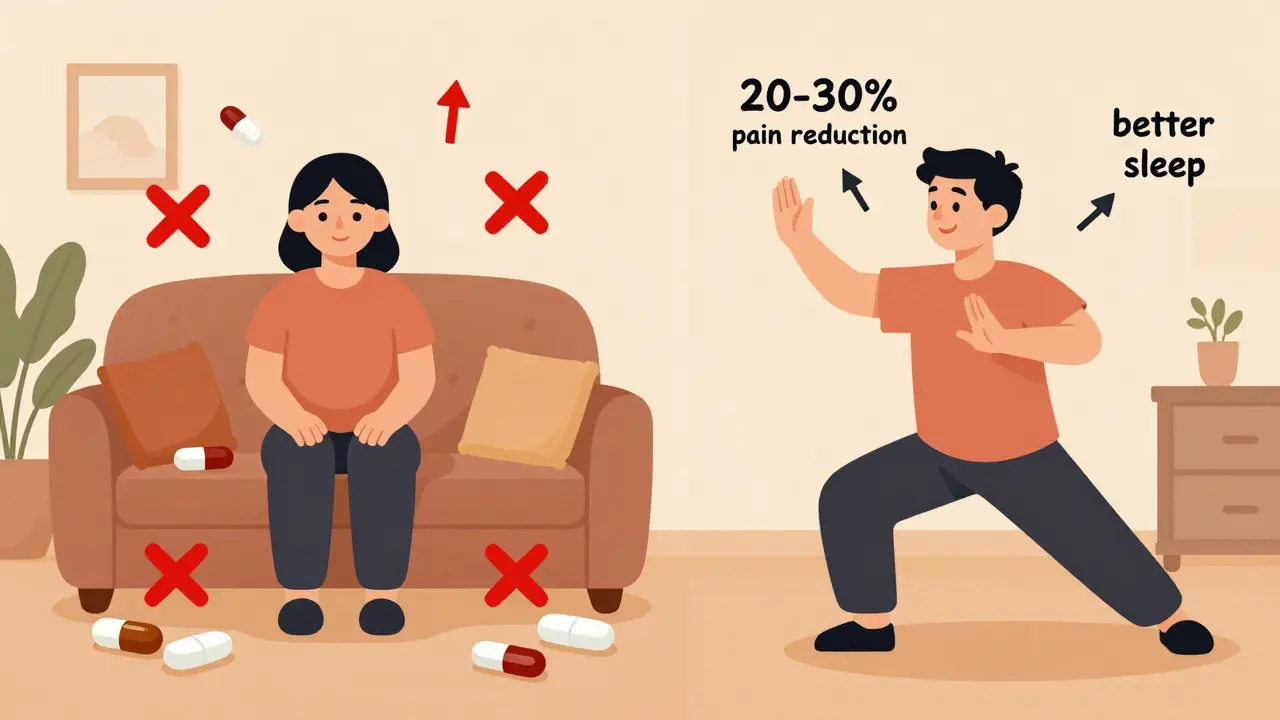
The Most Powerful Tool: Movement - Not Rest
It sounds backwards. When your body aches all the time, the instinct is to rest. But staying still makes fibromyalgia worse. The strongest evidence we have points to one thing: regular, gentle movement.
Start small. Walk for five minutes, two or three times a week. Swim. Ride a stationary bike. Do water aerobics. The goal isn’t to push through pain - it’s to move just enough to keep your muscles and nerves from stiffening up. Over 8 to 12 weeks, work up to 30 minutes, five days a week.
Studies show people who stick with aerobic exercise for 12 weeks see a 20-30% drop in pain. That’s better than most drugs. Strength training helps too, but aerobic activity wins when it comes to reducing pain intensity. One Cochrane review found aerobic exercise reduced pain by nearly a full point more on a 10-point scale than no exercise at all.
Start slow. If you feel worse after your first walk, don’t give up. That’s normal. It’s not your body breaking down - it’s your nervous system adjusting. Cut the time in half next time. Go every other day. Build up gradually. People on Reddit and MyFibroTeam report that after 6 months of consistent walking or swimming, their pain scores dropped from 8/10 to 4/10.
Cognitive Behavioral Therapy: Rewiring Your Brain’s Pain Response
CBT isn’t about "thinking positive." It’s about learning practical tools to break the cycle of pain, fear, and avoidance. When you hurt, you stop doing things. That leads to stiffness, weakness, and more pain. CBT teaches you how to pace yourself, challenge catastrophic thoughts (like "I’ll never get better"), and manage flare-ups without panic.
A 2010 meta-analysis found CBT reduced pain intensity by 25-30% - better than relaxation techniques alone. People who did CBT also reported less anxiety and better sleep. The structure is usually 8 to 12 weekly sessions with a trained therapist.
The problem? Insurance often won’t cover it. One in two patients say they’ve struggled to find a therapist who accepts their plan. Online programs like those offered by the Arthritis Foundation or through telehealth platforms are helping close that gap. Reddit users give CBT tools a 4.2 out of 5 rating, especially praising the "flare-up playbook" - a set of steps to follow when symptoms spike.
What Works (and What Doesn’t) in Complementary Therapies
More than half of people with fibromyalgia try something beyond meds and exercise. Some help. Some don’t. Here’s what the data says:
- Tai chi: Practiced twice a week for 12 weeks, it improved pain and function in multiple studies. One patient said it let them cut their medication in half.
- Yoga and massage: Popular and widely used. Yoga improves flexibility and reduces stress. Massage can ease muscle tension, though effects are often short-term.
- Acupuncture: Some feel better after sessions, but high-quality studies show it’s no better than fake acupuncture. The relief might come from the ritual, not the needles.
- Myofascial release: A form of deep tissue massage. One study showed a 22% improvement in quality of life after 12 weekly sessions.
Don’t waste money on expensive supplements or unproven devices. Stick with what’s been tested: movement, mindfulness, and touch therapies that feel good without breaking the bank.
Living With Flare-Ups - The Real Daily Battle
Nearly 9 out of 10 people with fibromyalgia deal with flare-ups. They can be triggered by stress, bad sleep, weather changes, or even too much activity the day before. The key isn’t to avoid them - it’s to manage them without letting them take over.
Learn pacing. Break tasks into tiny pieces. Do 10 minutes of laundry, then sit down. Walk for 5 minutes, rest for 15. Keep a journal to spot your triggers. Was it the late night? The argument? The rain? Knowing what sets off your flare helps you plan around it.
Also, stop thinking of rest as lazy. Rest is part of the treatment. On bad days, skip the walk. Take a nap. Drink water. Listen to calming music. Pushing through pain just makes the flare last longer.
Building a Support System - You Don’t Have to Do This Alone
Fibromyalgia can feel isolating. Friends don’t get it. Family thinks you’re exaggerating. Work doesn’t understand why you need to leave early. That’s why finding your people matters.
Online communities like FibroCenter or MyFibroTeam have thousands of active members sharing tips, venting, and celebrating small wins. The Arthritis Foundation runs local exercise classes tailored for chronic pain. You don’t need to be an athlete - you just need to show up.
Also, talk to your doctor about pain neuroscience education (PNE). It’s a simple concept: your brain is overreacting to harmless signals. When you understand that, you stop blaming your body. Studies show people who learn PNE stick to their treatment plans 35% more often.
What’s Next? Hope on the Horizon
Research is moving fast. The NIH spent $18.7 million in 2023 on fibromyalgia studies, focusing on brain imaging and new non-opioid pain drugs. A new medication called NBI-1117568 is showing promise in early trials, with 35% pain reduction in some patients.
But the biggest shift isn’t in labs - it’s in mindset. Doctors are finally listening. Guidelines from the European League Against Rheumatism now call exercise a "first-line treatment." The American College of Rheumatology says CBT and movement are more important than pills.
There’s no cure yet. But there’s a path - and it’s not about becoming pain-free. It’s about becoming less controlled by pain. You can still travel, work, laugh, and enjoy life. It just looks different now. And that’s okay.
Can fibromyalgia go away on its own?
Fibromyalgia doesn’t usually disappear completely. But symptoms can improve significantly with consistent lifestyle changes. Many people reach a point where their pain is manageable enough to live full, active lives. It’s not about waiting for it to vanish - it’s about building habits that reduce its grip on you.
Is it safe to take painkillers like ibuprofen for fibromyalgia?
Over-the-counter painkillers like ibuprofen or acetaminophen rarely help fibromyalgia pain because it’s not caused by inflammation. They might help with occasional headaches or muscle soreness from other causes, but they won’t touch the core nerve-related pain. Long-term use can also harm your stomach or kidneys. Stick to treatments proven for fibromyalgia.
How long does it take to see results from exercise or CBT?
You might feel a little better after 4-6 weeks, but real progress takes time. Most studies show noticeable improvements after 12 weeks of consistent exercise or CBT. The key is persistence. If you stop after a month, you won’t see results. Think of it like brushing your teeth - it’s not a quick fix, it’s daily maintenance.
Why do some doctors still push opioids for fibromyalgia?
Some doctors still prescribe opioids out of habit or because they feel pressured by patients in pain. But major guidelines from the European League Against Rheumatism and the CDC strongly advise against them. Opioids don’t work well for fibromyalgia, carry a high risk of dependence, and can actually make pain worse over time. Stick with evidence-based treatments.
Can stress make fibromyalgia worse?
Yes - and not just emotional stress. Physical stress like poor sleep, illness, or even too much activity can trigger flare-ups. That’s why CBT and mindfulness practices are so important. They help your nervous system calm down. Simple breathing exercises, journaling, or even a daily walk in nature can reduce your overall stress load and lead to fewer flares.
Should I stop working if I have fibromyalgia?
Most people with fibromyalgia can keep working - but they may need adjustments. Talk to your employer about flexible hours, remote work options, or taking short breaks. Many find that a structured routine helps them manage symptoms better than being home all day. If your job is physically demanding, consider switching roles or asking for accommodations. You don’t have to quit - you just might need to adapt.
Final Thought: It’s About Progress, Not Perfection
You won’t wake up one day pain-free. But you can wake up feeling more in control. One small walk. One session of CBT. One day where you didn’t beat yourself up for resting. Those add up. Fibromyalgia changes your life - but it doesn’t have to define it. Keep going. Even on the hard days. Progress isn’t linear. But it’s real.
15 Comments
Sophie Stallkind
December 26, 2025 AT 01:59 AM
The evidence supporting aerobic exercise as a first-line intervention is robust and clinically significant. It is imperative that patients understand that movement, even in minimal doses, modulates central sensitization through neuroplastic mechanisms. Rest is not therapeutic; it is counterproductive.
sagar patel
December 27, 2025 AT 13:13 PM
You say movement helps but you dont say how much is too much. I did 20 mins walk and was bedridden for 3 days. This advice is dangerous if you dont give limits.
Bailey Adkison
December 27, 2025 AT 23:49 PM
Of course exercise works. Just like how eating vegetables cures cancer. People want simple answers so they ignore the fact that fibro is a catch-all dumpster fire for doctors who dont know what else to call it.
Mussin Machhour
December 29, 2025 AT 08:17 AM
I was skeptical too but I started with 5 minute walks every other day. Now I do 30 min daily. It didn't fix me but it gave me my life back. You don't need to be strong. You just need to show up.
Lindsay Hensel
December 30, 2025 AT 17:12 PM
I wept reading this. After 12 years of being told it was all in my head, this is the first time I’ve seen someone articulate what I live with. Thank you.
Ben Harris
December 31, 2025 AT 04:01 AM
I did CBT and it made me feel worse because it made me feel guilty for being in pain. Like I was choosing to suffer. So I stopped. And guess what? I still have fibro. But now I’m not ashamed of it.
Oluwatosin Ayodele
December 31, 2025 AT 07:43 AM
You mention tai chi but ignore that it is a spiritual practice rooted in Taoist philosophy. The real benefit is not biomechanical but energetic. Western medicine ignores qi. That’s why their studies are flawed.
Winni Victor
January 1, 2026 AT 11:04 AM
Oh great. Another post telling me to walk it off like I’m some kind of lazy sloth who just needs to try harder. Meanwhile my joints feel like they’re filled with ground glass and my brain is a fog machine on full blast. Thanks for the guilt trip.
Rick Kimberly
January 2, 2026 AT 00:25 AM
The NIH funding increase is encouraging. However, the methodological limitations of current CBT trials-particularly the lack of active control groups and long-term follow-up-warrant caution in overgeneralizing outcomes.
Terry Free
January 2, 2026 AT 18:41 PM
Medications work? Sure. If you’re okay with dizziness, nausea, and becoming a walking zombie. Meanwhile the real solution is just saying no to modern life. Sleep. Quiet. No screens. No stress. But who has time for that?
Michael Dillon
January 4, 2026 AT 08:00 AM
I tried acupuncture. Felt nothing. Then I tried fake acupuncture with toothpicks. Same result. So yeah, placebo. But hey, if it makes people feel better, who am I to judge? Just don’t pay $150 for it.
Jason Jasper
January 4, 2026 AT 21:09 PM
I’ve been doing water aerobics twice a week for a year. It’s not glamorous. No one posts about it. But it’s the only thing that lets me get dressed without crying. I don’t need a trophy. I just need to not be broken.
Carlos Narvaez
January 6, 2026 AT 16:40 PM
Pregabalin is overrated. I took it for six months. Weight gain, brain fog, zero pain relief. Now I use CBD oil. It’s not FDA-approved but it’s real. And it works.
Harbans Singh
January 6, 2026 AT 17:41 PM
Hey, I’m from India and we have a lot of people here with fibro too. I started with 10 minutes of stretching in the morning. Now I teach it to others. You don’t need fancy gear. Just your body and patience. We’re all in this together.






Katherine Blumhardt
December 24, 2025 AT 16:24 PM
I tried yoga for 3 months and my pain went from 9/10 to 5/10. Not magic, just consistency. I still have bad days but now I know how to ride them out.