
Opioid Dose Adjustment Calculator for Older Adults
Calculate Safe Opioid Dose
Based on CDC and American Geriatrics Society guidelines for older adults (65+)
Older adults are more likely to take opioids for chronic pain - but they’re also far more likely to suffer serious side effects like falls, confusion, and even death. It’s not just about taking a pill. It’s about how the body changes with age, how other medications interact, and how easily these dangers go unnoticed. Many doctors still prescribe opioids the same way they would for a 40-year-old, even though an 80-year-old processes drugs completely differently. The result? Emergency rooms see more older adults than ever before because of opioid-related problems - and too often, it’s too late by the time someone realizes what’s happening.
Why Older Bodies React Differently to Opioids
Your liver and kidneys don’t work as fast after 65. Your body fat increases, muscle mass decreases, and the barrier that protects your brain from toxins becomes more porous. That means even a small dose of an opioid - say, oxycodone or tramadol - can build up in your system faster and hit your brain harder than it would in a younger person. A dose that’s perfectly safe for someone in their 50s might leave an older adult drowsy, dizzy, or confused.
Studies show that older adults are up to twice as likely to die from opioid-related causes compared to younger people with the same condition. This isn’t just about addiction. It’s about how the body breaks down drugs. When kidneys slow down, opioids stick around longer. When liver enzymes weaken, the body can’t clear them efficiently. And if you’re already taking blood pressure pills, antidepressants, or sleep aids, those can mix with opioids and make sedation worse - sometimes dangerously so.
Falls Aren’t Just Accidents - They’re a Red Flag
If an older adult falls once, it’s a warning. If they fall twice, it’s a crisis. And opioids are one of the top reasons why. These drugs don’t just make you sleepy. They lower your blood pressure when you stand up, blur your vision, slow your reaction time, and throw off your balance. Even weak opioids like tramadol can cause hyponatremia - low sodium - which leads to dizziness, nausea, and confusion. All of that adds up to a much higher chance of hitting the floor.
One study of over 2,300 adults over 60 found that those taking opioids had a 28% higher chance of breaking a bone over three years. That’s not a small risk. Hip fractures in older adults often lead to long-term disability, nursing home stays, or death. And it’s not just about the fall itself - it’s about what happens after. Recovery is slower. Complications are more common. Many people never regain their independence.
Delirium: The Silent Danger No One Talks About
Delirium - sudden confusion, disorientation, hallucinations - is often mistaken for dementia or just "getting older." But in older adults, it’s frequently triggered by medications. Opioids are a major culprit. Even short-term use can cause acute delirium, especially in those with early memory problems or existing brain changes.
A 2023 study from Denmark tracked over 75,000 older adults with dementia. Those who started opioids had an elevenfold increase in death risk during the first two weeks. That’s not a typo. Eleven times more likely to die. And most of these patients weren’t even prescribed opioids for cancer pain - they were getting them for arthritis or back pain. Doctors didn’t realize how quickly these drugs could push someone into delirium, and families didn’t know to connect the dots between a new prescription and sudden confusion.
The problem? Delirium often looks like normal aging. A grandparent becomes quieter. Stops recognizing people. Doesn’t eat. The family thinks it’s just dementia getting worse. But it might be the opioid. And if it’s caught early, stopping the drug can reverse it.

How to Adjust Doses - Start Low, Go Slow
There’s no one-size-fits-all dose for older adults. But there is one rule that saves lives: start low, go slow.
- Begin with 25% to 50% of the dose you’d give a younger adult.
- Wait at least 5-7 days before increasing it - longer if the person has kidney or liver issues.
- Use immediate-release forms, not long-acting ones, unless absolutely necessary.
- Avoid tramadol in people over 75 - it’s linked to more falls and hyponatremia.
- Never combine opioids with benzodiazepines, sleep meds, or muscle relaxants without extreme caution.
Many doctors still default to standard dosing because they’re not trained in geriatric pharmacology. But guidelines from the CDC, the American Geriatrics Society, and the STOPPFall tool all agree: lower doses are safer. And if pain isn’t improving after a week at a low dose, the opioid probably isn’t helping - and the risks are mounting.
Deprescribing Is Not Giving Up - It’s Saving Lives
Stopping opioids isn’t easy. Many older adults have been on them for years. They fear the pain will come back. They worry their doctor thinks they’re weak. But staying on opioids long-term often makes pain worse over time - a condition called opioid-induced hyperalgesia.
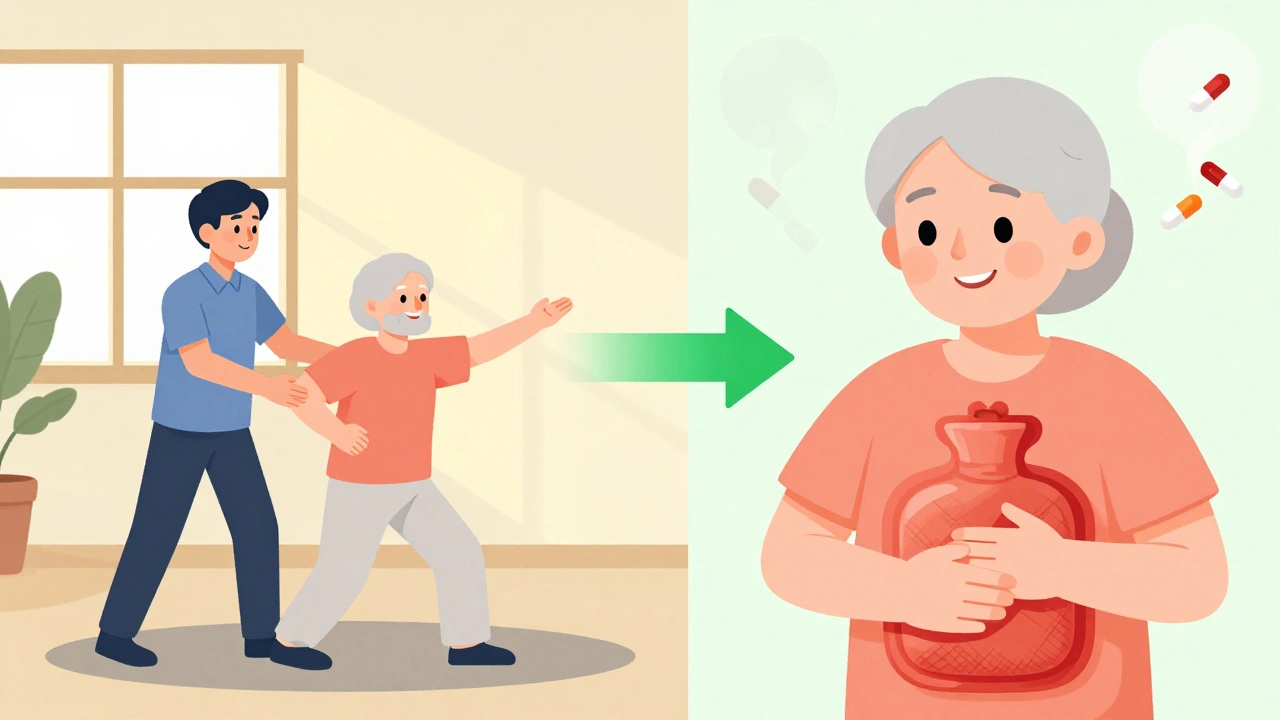
Deprescribing means slowly lowering the dose while watching for withdrawal signs: sweating, anxiety, nausea, trouble sleeping. It’s not about cutting cold turkey. It’s about switching to safer alternatives - physical therapy, heat packs, acupuncture, nerve blocks, or non-opioid pain relievers like acetaminophen (with caution for liver issues).
The STOPPFall tool helps doctors decide when to reduce or stop opioids in people who’ve fallen or are at risk. It’s not a checklist - it’s a conversation starter. It asks: Is this drug doing more harm than good? Are there other ways to manage pain? Has the patient’s balance gotten worse? Has their mind changed?
The Communication Gap Between Doctors and Patients
Doctors are more worried about falls and confusion. Older adults are more worried about addiction. But few ever talk about both.
One study found nearly half of primary care doctors didn’t feel confident helping patients taper off opioids. And many older adults didn’t know they could become physically dependent in just a few days - or that withdrawal isn’t the same as addiction. They think addiction means stealing pills or lying to get more. But physical dependence? That’s just your body adapting. It’s normal. And it’s manageable.
Trust is the missing piece. If a patient doesn’t feel heard, they won’t agree to stop. If a doctor doesn’t explain the risks clearly, the patient won’t understand why. The best conversations happen when doctors say: "I’m not taking this away because I think you’re weak. I’m adjusting it because I care about your safety. Let’s find a way to keep you mobile and pain-free without putting you at risk."
What Families Can Do
If you’re caring for an older relative on opioids, here’s what to watch for:
- Do they seem more confused than usual after a new prescription?
- Have they fallen recently - even once?
- Do they sleep more, move slower, or stop talking as much?
- Are they taking more than one pain medication?
Keep a list of all their medications - including over-the-counter ones - and bring it to every doctor visit. Ask: "Could this medicine be making them more dizzy or confused?" Don’t assume the doctor knows. Many don’t.
And if your loved one is on opioids for chronic pain that hasn’t improved in months - ask about alternatives. There are better, safer ways to manage pain in older adults. Opioids shouldn’t be the first or only option.
The Future of Pain Management for Older Adults
The tide is turning. More doctors are learning about geriatric pain. More guidelines are being updated. More tools like STOPPFall are being used in clinics. Non-drug treatments - tai chi, physical therapy, cognitive behavioral therapy - are proving just as effective as opioids for many types of pain, without the risks.
But the legacy of overprescribing won’t disappear overnight. Thousands of older adults are still on opioids they don’t need, and many doctors still see them as the only answer. The key is awareness. If you’re over 65 and on opioids, ask: "Is this still helping? Are there safer options?" If you’re a caregiver, speak up. These drugs aren’t harmless. They’re dangerous - especially when no one’s watching.
10 Comments
Chris Park
December 6, 2025 AT 09:21 AM
Interesting. But have you considered that the CDC guidelines were influenced by pharmaceutical lobbying disguised as "evidence-based practice"? The 28% higher fracture risk? Correlation ≠ causation. What about the unmeasured confounders - polypharmacy from non-opioid drugs, vitamin D deficiency, lack of sunlight, or even 5G-induced neurotoxicity? The real epidemic is not opioids - it’s the erosion of bodily autonomy under paternalistic medical dogma. They call it "deprescribing." I call it chemical control.
Saketh Sai Rachapudi
December 6, 2025 AT 12:17 PM
OMG this is so true!!! I saw my uncle on tramadol for back pain and he started talking to the TV like it was his dead wife!! And the doctor just said "oh he's getting old" NOOOO it's the drugs!! We need to ban opioids for anyone over 60!! Why are doctors still prescribing this crap?? My aunt fell and broke her hip and now she's in a nursing home and it's ALL because of these pills!!! Someone needs to go to jail for this!!!
joanne humphreys
December 8, 2025 AT 05:48 AM
This is one of the most important pieces I’ve read this year. The way delirium is dismissed as "just dementia" is horrifying. I had a neighbor who became withdrawn after starting oxycodone for arthritis. We didn’t realize it was the medication until she stopped taking it - and within two weeks, she was back to telling stories from her childhood, recognizing everyone, even laughing again. It wasn’t dementia. It was reversible. We need more doctors who listen - not just prescribe.
Nigel ntini
December 8, 2025 AT 20:29 PM
Well said. The "start low, go slow" principle isn’t just medical advice - it’s a philosophy of care. Too many clinicians treat aging like a bug to be fixed, not a stage of life to be honored. I’ve seen patients thrive after switching to tai chi and acupuncture. Their pain didn’t vanish - but their dignity did. And that’s worth more than any pill. Keep pushing this message. The system needs more voices like yours.
Priya Ranjan
December 9, 2025 AT 19:49 PM
It’s pathetic. People over 65 should not be allowed to take opioids at all. They’re a burden on the system, emotionally and financially. If you can’t handle pain without drugs, maybe you shouldn’t be living independently. My mother took acetaminophen and prayed - and she lived to 92. No falls. No confusion. Just discipline. This isn’t medicine - it’s weakness dressed up as compassion.
Gwyneth Agnes
December 11, 2025 AT 02:17 AM
Opioids kill older people. Stop prescribing them.
Ashish Vazirani
December 12, 2025 AT 07:26 AM
THIS. IS. A. CRIME. I saw my grandfather - a war veteran - go from sharp as a tack to a shell of a man in three weeks after they gave him tramadol for "mild sciatica." He stopped eating. Stopped talking. Started calling his dead wife by my name. We begged the doctor to stop it. He said, "It’s just a small dose." Small dose? It killed his mind. Now he’s in a home. And the doctor? Got a bonus for hitting his pain management targets. This isn’t healthcare. It’s a slaughterhouse with a stethoscope.
Mansi Bansal
December 14, 2025 AT 02:50 AM
While the clinical rationale presented herein is both methodologically sound and empirically corroborated, one cannot overlook the sociocultural dissonance inherent in the contemporary pharmacological paradigm. The normalization of opioid prescription in geriatric populations reflects a systemic devaluation of non-pharmaceutical modalities - a trend exacerbated by institutional inertia and the commodification of patient care. It is not merely a matter of dosage adjustment, but of epistemological reorientation: from reductionist pharmacology to holistic gerontology. The STOPPFall tool, while commendable, remains insufficient without concurrent policy reform and physician re-education.
Max Manoles
December 14, 2025 AT 15:35 PM
My grandmother was on opioids for five years after a hip replacement. We thought it was helping - until she started forgetting how to button her coat. We tapered her off slowly with her pain specialist’s help. Six months later, she was walking without a cane, sleeping through the night, and even joined a book club. It wasn’t magic. It was just removing something that was quietly stealing her life. If you’re on opioids and feel like you’re fading - it’s not aging. It’s the drug. Ask for help. You’re not weak for wanting to feel like yourself again.






Mayur Panchamia
December 5, 2025 AT 12:54 PM
Let’s be real - this isn’t about "safe dosing," it’s about Western medicine’s obsession with pills over discipline! In India, grandmas manage chronic pain with turmeric paste, yoga, and a stern look. No opioids. No hospital trips. Just wisdom passed down through generations. Why are we outsourcing common sense to Big Pharma? The system is broken - and it’s not because older bodies are fragile, it’s because we’ve forgotten how to live!