
When your MS symptoms suddenly get worse, it’s natural to panic. Is this a relapse? Did the disease suddenly flare up again? Or is it something else-something temporary, something you can fix without drugs? The difference between a true MS relapse and a pseudorelapse isn’t just medical jargon. It’s the difference between getting IV steroids and avoiding them altogether. And getting it wrong can mean unnecessary side effects, higher costs, and even serious complications like steroid-induced psychosis.
What’s Really Happening: Relapse vs. Pseudorelapse
A true MS relapse happens when your immune system attacks your central nervous system again. New inflammation damages the myelin sheath around nerves. That’s what causes new symptoms-or makes old ones much worse. These symptoms last at least 24 to 48 hours, and they’re not tied to anything like a fever or a hot shower. If you’ve had numbness in your leg before, and now it’s spreading to your whole side, and it’s been going on for two days with no obvious reason, that’s likely a relapse. A pseudorelapse is different. It’s not new damage. It’s old damage acting up. Think of it like a frayed wire that works fine until it gets too hot. When your body temperature rises-even by a degree or two-nerves that are already damaged by MS can’t send signals properly. Your symptoms get worse, but your brain and spinal cord aren’t getting hit by new inflammation. Once the trigger is gone, so are the symptoms. This is called Uhthoff’s phenomenon when heat causes vision problems. Around 60 to 80% of people with MS who’ve had optic neuritis experience this.What Triggers a Pseudorelapse?
Pseudorelapses aren’t random. They’re tied to specific, often avoidable, triggers. The most common one? Urinary tract infections (UTIs). In fact, about 67% of pseudorelapses are linked to infections, and UTIs make up the biggest chunk. If you’ve had a sudden spike in bladder issues, fatigue, or leg weakness-and you haven’t had a relapse in months-check for a UTI. A simple urine test can confirm it. Heat is another big one. A hot bath, a sauna, even a hot day outside can trigger symptoms. You might notice your vision blurring, your legs feeling heavy, or your balance getting worse. It’s not the heat causing damage-it’s just making your damaged nerves work even harder. Cooling down, even with a fan or a cooling vest, can reverse the symptoms in minutes to hours. Other triggers include:- Fever from a cold or flu (32% of cases)
- Physical exhaustion or overexertion (28%)
- High stress levels (19%)
- Electrolyte imbalances like low sodium
When Steroids Are-and Aren’t-Used
Steroids like high-dose IV methylprednisolone are the standard treatment for true relapses. They reduce inflammation, speed up recovery, and help you get back to normal faster. About 70 to 80% of people see improvement within days. But steroids don’t fix pseudorelapses. Why? Because there’s no inflammation to fight. Giving steroids for a pseudorelapse doesn’t help. It just adds risk. Around 25% of patients develop high blood sugar. 40% get severe insomnia. 30% feel anxious or depressed. And since steroids weaken your immune system, you’re more likely to get worse infections. One nurse on Reddit shared that five patients she saw in a year got unnecessary IV steroids for UTI-triggered pseudorelapses. One ended up in the hospital with steroid-induced psychosis. The American Academy of Neurology says: Before you treat a relapse, rule out triggers. Check for fever. Test for UTIs. Look at your sodium levels. If you find a trigger, treat that-don’t reach for the steroids. Only if symptoms last more than 48 hours, and no trigger is found, should steroids be considered.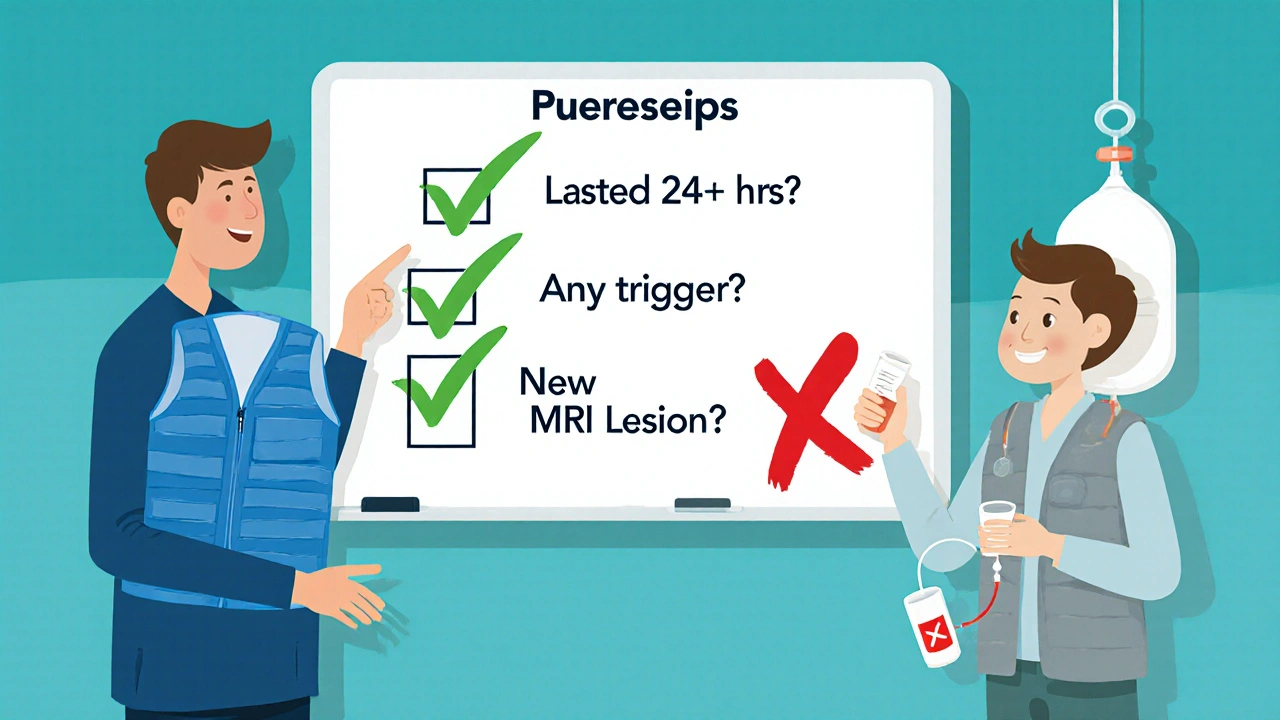
How Doctors Tell the Difference
Neurologists use a simple three-step checklist:- Did symptoms last more than 24 hours?
- Is there a clear trigger (infection, heat, stress)?
- Is there new damage on an MRI?
Who’s Most at Risk for Pseudorelapses?
You’re more likely to have pseudorelapses if you’ve had MS for a long time. As the disease progresses, you accumulate more nerve damage. That means more pathways are vulnerable to heat, fatigue, or infection. Older patients, especially over 55, are also more likely to have lasting functional changes after a pseudorelapse-not because of new damage, but because their bodies take longer to recover from the strain. About 15% of older patients don’t fully bounce back after a heat-triggered episode, even after cooling down. It’s also more common in people with higher disability scores. Someone who already uses a cane might notice their walking gets much worse during a UTI. That doesn’t mean the MS is getting worse. It means their body is already running on empty, and the infection pushed them over the edge.What You Can Do Right Now
You don’t need to wait for a flare-up to be prepared. Here’s what works:- Keep a symptom diary. Note temperature, sleep, stress, infections, and activity levels.
- Know your triggers. If heat makes you worse, avoid hot showers. Use cooling towels or vests in summer.
- Treat UTIs fast. If you have burning, urgency, or cloudy urine, get tested. Don’t wait.
- Don’t assume every symptom spike is a relapse. Ask: Did something change? Did I get sick? Did I overdo it?
- Ask your doctor about the MS-Relapse Assessment Tool (MS-RAT). It’s a new online tool that asks you questions about your symptoms and gives a probability score for relapse vs. pseudorelapse-with 92% accuracy.
The Bigger Picture
Misdiagnosing a pseudorelapse as a relapse isn’t just a mistake-it’s expensive. In the U.S. alone, unnecessary steroid treatments for pseudorelapses cost about $12.7 million a year. That’s money spent on hospital visits, IV drips, and managing side effects that could have been avoided. The good news? Awareness is growing. Telehealth platforms like MS Selfie are helping patients record symptoms and send them to specialists in real time. With better tools and better education, more people are learning to recognize pseudorelapses before they rush to the ER. The key takeaway? Not every worsening of symptoms means your MS is progressing. Sometimes, it’s just your body asking for rest, cool air, or a simple antibiotic. Knowing the difference gives you control. It keeps you from unnecessary treatments. And it helps you live better with MS-without fear of every little change being a disaster.How do I know if my symptoms are a relapse or a pseudorelapse?
Check for triggers first: Did you get sick? Are you overheated? Have you been stressed or exhausted? If yes, and your symptoms improve within hours after fixing the trigger, it’s likely a pseudorelapse. If symptoms last more than 48 hours with no clear cause, and you have new or worsening neurological signs, it’s probably a true relapse. An MRI can confirm new lesions if there’s still doubt.
Can pseudorelapses cause permanent damage?
No. Pseudorelapses don’t cause new nerve damage or lead to long-term disability. They’re temporary disruptions in nerve signaling due to existing damage. But in older or more disabled patients, the strain from a pseudorelapse can lead to temporary loss of function, like needing a walker for a few days after a UTI. That’s not progression-it’s deconditioning. Getting back to normal activity helps restore function.
Why do steroids work for relapses but not pseudorelapses?
Steroids reduce inflammation. True relapses involve active inflammation damaging nerves. Pseudorelapses involve no new inflammation-just existing damaged nerves struggling under stress. Giving steroids for pseudorelapses is like using a fire extinguisher on a power outage. It doesn’t fix the problem and can cause side effects like high blood sugar, insomnia, or mood swings.
What’s Uhthoff’s phenomenon, and how common is it?
Uhthoff’s phenomenon is a type of pseudorelapse where symptoms-usually vision problems-worsen with increased body temperature. It affects 60 to 80% of MS patients who’ve had optic neuritis. Symptoms improve within minutes to hours after cooling down. It’s not dangerous, but it’s a clear sign you’re sensitive to heat. Cooling vests, staying in air-conditioned spaces, and avoiding hot tubs help manage it.
Should I get an MRI every time my symptoms get worse?
No. MRIs are expensive and not always necessary. If your symptoms clearly match a trigger like heat or infection and improve quickly, you likely don’t need one. But if symptoms last over 48 hours, are new, or you’re unsure, an MRI can show whether there’s new inflammation. Your neurologist will decide based on your history and symptoms-not just because you’re worried.
Can stress really trigger a pseudorelapse?
Yes. Stress raises cortisol and body temperature slightly, and it can disrupt sleep and immune function. For someone with MS, that’s enough to overload already damaged nerves. Studies show stress triggers pseudorelapses in about 19% of cases. Managing stress with rest, breathing exercises, or counseling can help prevent these episodes.
Is there a test to confirm a pseudorelapse?
There’s no single blood test, but doctors use a combination: checking for fever, testing urine for infection, measuring sodium levels, and reviewing your symptom diary. The new MS-Relapse Assessment Tool (MS-RAT) uses your answers to questions about duration, triggers, and function to give a probability score. It’s 92% accurate at distinguishing relapses from pseudorelapses.
8 Comments
Kihya Beitz
November 16, 2025 AT 07:59 AM
Oh wow, another ‘MS guide’ that sounds like it was written by a pharma rep who got paid to say ‘steroids bad’.
Let me guess - next you’ll tell us not to breathe because oxygen causes inflammation? 😒
Meanwhile, my neurologist just shrugs and hands me a prescription like it’s a vending machine.
Thanks for the ‘awareness’… I’ll stick with my gut and my ER visits.
Hollis Hollywood
November 18, 2025 AT 02:59 AM
I’ve been living with MS for 14 years, and I can’t tell you how many times I’ve panicked thinking I was having a relapse - only to realize it was a UTI or a too-hot shower. I keep a little thermometer and a symptom log in my phone now. It’s saved me from two unnecessary steroid courses.
One time, I had this weird leg weakness for three days. I thought I was doomed. Then I remembered I’d been running a low-grade fever from a sinus infection. Once the infection cleared, the weakness vanished in 18 hours. No MRI. No IV. Just rest and antibiotics.
It’s not that relapses aren’t real - they are. But so many of us are scared into thinking every twitch is the end. We need to learn the difference, not just fear it.
And yeah, steroids? They’re not harmless. I had insomnia for weeks after one course. Felt like I was living inside a buzzing fluorescent light. Not worth it if you don’t need it.
Aidan McCord-Amasis
November 18, 2025 AT 08:40 AM
Heat = bad. UTIs = sneaky. Steroids = overkill. 🚫💊
Diary = your new best friend. 📓
Stop panicking. Start tracking.
Ogonna Igbo
November 19, 2025 AT 08:50 AM
You people in America and Canada think you have monopoly on medical knowledge. In Nigeria we don't have MRI machines every corner but we know when it's infection or heat. We don't need fancy tools. We know our bodies. We don't rush to steroids because we know our children are dying from malaria and cholera and you are worrying about side effects of medicine you don't even need. Your system is broken. You treat symptoms like enemies not signs. You have money to waste. We have survival to fight. Your MS is not a luxury problem. It's a global problem. Stop acting like you are the only ones who suffer.
And yes we have MS too. We just don't have time to write long blogs about it.
BABA SABKA
November 20, 2025 AT 19:25 PM
Let’s cut through the noise. Pseudorelapses are neurophysiological noise - not disease progression. The CNS is a high-impedance circuit. When demyelinated axons get thermally or metabolically stressed, conduction blocks occur. No new lesion? No immune activation? Then it’s not a relapse. It’s a transient signal failure.
And yes - UTIs are the #1 trigger because systemic inflammation elevates core temp and alters sodium-potassium gradients. Cortisol spikes from stress? Same mechanism. Steroids don’t fix conduction blocks. They suppress immune pathways that aren’t even active. That’s why they’re not just ineffective - they’re counterproductive.
MS-RAT? Finally. A tool that doesn’t treat MS like a black box. We need more of this. Not more MRIs. More phenomenology.
Also - cooling vests? Non-negotiable. I wear mine to the grocery store in July. People stare. I don’t care.
Chris Bryan
November 21, 2025 AT 03:21 AM
Who funded this article? Big Pharma? The steroid manufacturers? They make billions off unnecessary IV drips. Did you know the FDA approved methylprednisolone for MS relapses in 1993 - but never required long-term safety studies? That’s because they knew it was a cash cow.
And now you’re telling us to avoid steroids? Too late. They’ve already hooked us. Your ‘MS-RAT’? A distraction. They want you to think you’re in control. But you’re still a patient. Still dependent. Still paying.
Why don’t they just admit they profit from fear? You don’t need a diary. You need to stop trusting the system.
They’ll keep giving you steroids until you’re too weak to fight back. Then they’ll say ‘your disease progressed’.
Wake up.
Jonathan Dobey
November 21, 2025 AT 04:12 AM
Let’s be real - we’re not talking about medicine here. We’re talking about the metaphysics of suffering.
Relapse? Pseudorelapse? These are just labels we slap on the chaos of our broken biology to make it feel manageable. But the truth? The body doesn’t care about your diagnostic categories. It just screams.
When your nerves are frayed, every whisper of heat becomes a hurricane. Every infection, a siege. Every moment of stress, a crack in the dam.
Steroids? They’re not a cure - they’re a temporary truce with your own unraveling. A chemical ceasefire in a war you didn’t choose.
And yet… we cling to them. We beg for them. Because to admit it’s a pseudorelapse means accepting that your body is fragile, not broken - and that the real enemy isn’t inflammation, but the unbearable weight of simply being alive with this disease.
So yes - track your triggers. Cool your skin. Test your urine.
But don’t pretend knowledge is power.
It’s just a slightly less painful way to grieve.





Jennifer Walton
November 14, 2025 AT 18:15 PM
Heat makes everything worse. I learned this the hard way after a hot yoga class. Thought I was relapsing. Turned out I just needed a fan and a cold drink. No steroids. No drama.
Simple fixes work.