
By 2025, if you’re waiting for a generic version of a brand-name drug like Eliquis or Xarelto, you’re not alone. The FDA approved these generics - sometimes over a year ago - but you still can’t buy them at your local pharmacy. Why? Because patent lawsuits, not safety issues or supply chains, are holding them back. It’s not a glitch. It’s the system.
How Patents Block Generic Drugs After FDA Approval
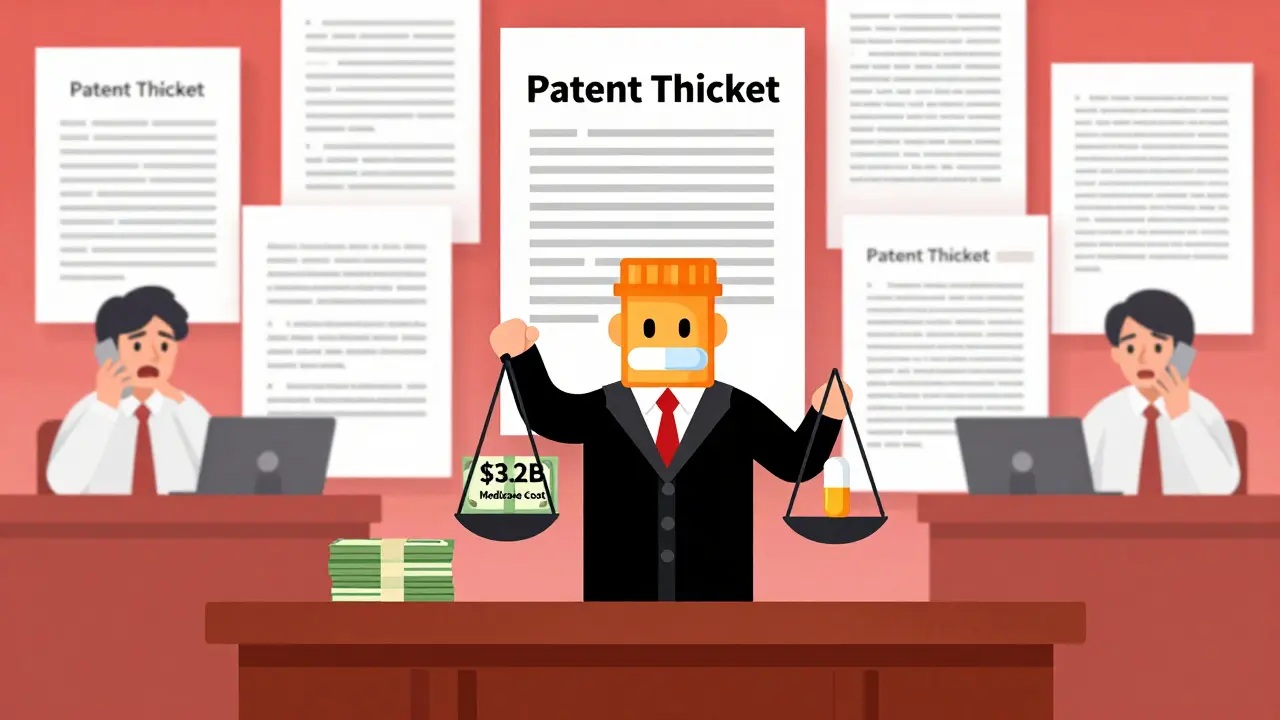
The FDA doesn’t control when a generic drug hits the market. Once a generic company files an application and says a patent is invalid or won’t be infringed (called a Paragraph IV certification), the brand-name company can sue. That triggers a 30-month automatic stay. The FDA can’t give final approval until that clock runs out - even if the patent is weak, outdated, or clearly meant to delay competition.
In 2024, 68% of all generic applications included this kind of patent challenge. By 2025, the average New Drug Application listed 14.7 patents. That’s up from 12.3 in 2020. These aren’t all strong patents. Many are minor tweaks - new dosages, delivery methods, or formulations - filed just before the main patent expires. This tactic, called patent thicketing, has become standard. One drug, Humira, had over 240 patents listed. That stretched its monopoly past 10 years, even though the core patent expired in 2016.
Real Examples: What’s Been Delayed (2023-2025)
Let’s look at what’s actually happening on the ground.
In 2023, the FDA approved the first generic for Trulicity, a $4.3 billion diabetes drug. But the brand company, Eli Lilly, filed new patents covering delivery devices. The result? A 30-month delay. Patients still pay $900 a month for the brand. The generic? Still not available in 2025.
Steglatro, another diabetes drug, followed the same path. Generic approval came in late 2023. By mid-2025, it was still locked up in litigation. Pharmacists report patients skipping doses because they can’t afford the brand. One survey found 82% of pharmacists get asked weekly: “Why is this generic approved but not in stock?”
Oncology drugs are hit hardest. The average delay between FDA approval and market launch for cancer generics is 4.1 years. Compare that to 2.3 years for CNS drugs and 2.8 for heart meds. Why? Because complex injectables are harder to copy, and brand companies fight harder to protect high-margin drugs. Of the 15 oncology drugs in shortage between 2023 and 2025, 14 were injectables - and 89% of those delays were tied to patent fights.
Why the FDA Can’t Fix This
The FDA approves drugs based on safety and effectiveness. It doesn’t decide patent validity. That’s a court’s job. Even with new tools - like AI-assisted reviews that cut approval time by 22% for non-litigated cases - the agency is powerless against the 30-month stay.
Dr. Patrizia Cavazzoni, head of the FDA’s drug center, admitted in May 2025: “We’re working to increase transparency around patent listings to prevent evergreening.” But transparency doesn’t stop lawsuits. It just makes them more visible.
The FDA’s new National Priority Voucher program speeds up reviews for certain drugs - but only if they’re not caught in patent litigation. For generics stuck in court, it’s useless.
Supply Chains, Costs, and Patient Harm
Patents aren’t the only problem - but they’re the biggest. About 37% of delayed generics also faced supply chain issues, especially for injectables. But even those delays are often worse because patent fights prevent companies from starting production early.
The cost to patients is staggering. The average monthly price for a brand-name drug like Xarelto is $512. The projected generic price? $85. That’s a 79% drop. But because generics are blocked, Medicare Part D spent $3.2 billion extra in 2025 on drugs that should have had competition.
Patient advocacy groups documented 412 cases between 2023 and 2025 where people skipped doses or stopped treatment because they couldn’t afford the brand. One woman in Ohio told reporters she was rationing her Eliquis pills - one every other day - because the generic wasn’t available. She’s not an outlier.
Who’s Getting Hurt the Most
Big generic companies like Teva and Sandoz can afford multi-million-dollar lawsuits. They’ve diversified their active ingredient suppliers from an average of 1.8 in 2022 to 3.4 in 2025. They’ve got legal teams and deep pockets.
Smaller companies? Not so lucky. In 63% of delayed generic cases, the applicant had annual revenue under $500 million. Many of these companies go bankrupt before their case is resolved. That’s not innovation. It’s consolidation. The market is becoming a game only big players can afford to play.
What’s Changing? And What’s Not
Some things are shifting. The practice of brand companies launching their own “authorized generics” to crush competition has dropped from 28% in 2020 to just 12% in 2025. That’s a good sign - it means they’re relying more on legal tactics than market tactics.
But the legal tactics are getting more aggressive. The average number of patents challenged per biosimilar application jumped from 5.2 in 2020 to 9.7 in 2025. The Humira patent battle set a precedent: file enough patents, and you can delay competition for a decade.
Legislators are trying. The CREATES Act, which would force brand companies to provide samples for testing, passed the House in 2024 but stalled in the Senate in 2025. The FTC filed 7 enforcement actions against patent abuse between 2024 and 2025 - including one against Jazz Pharmaceuticals over Xyrem. They settled, requiring earlier generic entry. But that’s a case-by-case fix. It doesn’t change the system.
What’s Next? The Real Solution
The system was designed in 1984 with the Hatch-Waxman Act. Back then, patents were simpler. One drug, one main patent. Today? One drug, 15 patents. The law hasn’t kept up.
Experts agree: we need limits on how many patents can be listed per drug. Right now, there’s no cap. A 2025 McKinsey survey found 67% of industry stakeholders support a cap. But PhRMA, the drug industry’s main lobbying group, says it would hurt innovation.
They’re wrong. Innovation isn’t about extending monopolies. It’s about creating new medicines - not rebranding old ones. The real innovation is in making drugs affordable. Right now, the patent system is blocking that.
Until Congress reforms the rules - and the courts stop treating every minor patent as a valid shield - patients will keep paying more, pharmacists will keep fielding angry calls, and generics will keep sitting on shelves, approved but unavailable.
How Generic Companies Are Adapting
They’re playing the long game. Leading generic manufacturers now start patent research 48 to 60 months before a patent expires. They file citizen petitions to get improper patents removed from the FDA’s Orange Book. But the average time to resolve one of those petitions? 18.2 months. That’s longer than most drug reviews.
They’re also hiring more regulatory affairs staff. Training now takes 27 months to get good at patent linkage - up from 18 months in 2020. Legal costs per case? $12.7 million in 2025. That’s up from $9.3 million in 2023.
It’s not just about making drugs. It’s about surviving lawsuits.
Why are generic drugs approved but not available?
Even after the FDA approves a generic drug, it can’t be sold if a brand-name company files a patent lawsuit. That triggers a 30-month automatic delay, regardless of whether the patent is strong or weak. Many generics are approved but stuck in legal limbo for years.
What’s the average delay between FDA approval and generic launch?
As of 2025, the average delay is 3.2 years. For complex drugs like injectables or oncology treatments, it can stretch to 4.1 years. In Europe, the average is just 1.7 years - because their patent system doesn’t allow the same kind of litigation delays.
Which drugs are most affected by patent delays?
High-revenue drugs with complex formulations face the longest delays. Examples include Eliquis (apixaban), Xarelto (rivaroxaban), Trulicity (dulaglutide), and Steglatro (ertugliflozin). Oncology drugs, especially injectables, are hit hardest, with 89% of delays tied to patent litigation.
Can the FDA speed up generic approval?
The FDA can approve generics faster - and has cut review times by 22% for non-litigated cases using AI tools. But it cannot override patent lawsuits. The 30-month stay is a legal barrier, not a regulatory one. The FDA has no authority to force a generic to market during litigation.
Are biosimilars affected the same way?
Yes - even more so. Biosimilars face complex patent landscapes. For example, Humira had over 240 patents listed, creating a 10-year exclusivity period. The average number of patents challenged per biosimilar application rose from 5.2 in 2020 to 9.7 in 2025. While biosimilar approvals are increasing, litigation delays are still the main barrier to market entry.
What’s being done to fix this?
The FTC has filed enforcement actions against companies using patent thickets to block competition. The CREATES Act would require brand companies to provide samples for testing, but it stalled in Congress in 2025. Some experts are pushing for a cap on the number of patents per drug - currently, there’s no limit. Without legislative change, delays will keep rising.
13 Comments
Kevin Lopez
December 31, 2025 AT 17:56 PM
Paragraph IV certifications + 30-month stays = regulatory capture. The Hatch-Waxman Act was never meant to enable patent thicketing at scale. 14.7 patents per NDA? That’s not IP protection-it’s litigation arbitrage. The FTC’s 7 actions are band-aids on a hemorrhage.
Duncan Careless
December 31, 2025 AT 21:17 PM
Man, this is rough. I work in a pharmacy in Manchester and we get asked about this every single day. Patients cry. They’re choosing between insulin and their rent. I don’t know what to say anymore. The system’s broken. 🙏
Samar Khan
January 2, 2026 AT 05:12 AM
OMG I CAN’T EVEN 😭 My dad’s on Xarelto and he skipped doses for 3 months because he couldn’t afford it. He had a mini-stroke. Now he’s on Medicaid. This isn’t healthcare. It’s extortion. 💔 #PharmaMurder
Russell Thomas
January 3, 2026 AT 12:31 PM
Oh wow, so the FDA approves drugs but the courts get to decide if they can be sold? That’s like letting a car company sue you for buying a used tire. Brilliant. Let’s just hand them the whole damn highway and call it ‘innovation.’ 🙃
Joe Kwon
January 3, 2026 AT 23:32 PM
There’s a middle ground here. We need to protect genuine innovation, but patent thickets are a loophole, not a feature. The CREATES Act could’ve helped, but it died because lobbying > public health. Maybe we need a patient-led coalition? I’m in if anyone’s organizing.
Nicole K.
January 4, 2026 AT 02:55 AM
People who support generics are just enabling laziness. If you can’t afford medicine, you shouldn’t be taking it. Maybe you should get a better job. This isn’t a right-it’s a privilege.
Fabian Riewe
January 4, 2026 AT 10:14 AM
Hey, I’ve been in pharma for 18 years. I’ve seen this cycle before. The good news? Generic companies are getting smarter. They’re filing citizen petitions, diversifying suppliers, training staff for 2+ years just to navigate the mess. It’s a war, but they’re not giving up. Hope isn’t dead-it’s just really tired.
Amy Cannon
January 4, 2026 AT 23:40 PM
It is of paramount importance to recognize that the structural inefficiencies embedded within the United States pharmaceutical patent regime represent a profound dissonance between statutory intent and contemporary corporate practice. The Hatch-Waxman Act, enacted in the 1980s, was predicated upon a paradigm of singular patent protection, whereas the current milieu of 14.7 patents per NDA constitutes a systemic perversion of legislative purpose. Moreover, the 30-month stay, while ostensibly a procedural safeguard, has metastasized into a de facto market exclusivity extension mechanism, thereby undermining the foundational ethos of affordable access. One might posit that legislative reform must be both targeted and unyielding-perhaps a cap of five patents per drug, with mandatory public disclosure of all patent claims within 30 days of submission. Alas, the lobbying apparatus remains formidable, and the moral imperative remains unmet.
Greg Quinn
January 5, 2026 AT 08:39 AM
It’s funny how we call this ‘innovation’ when it’s really just legal engineering. We’ve turned medicine into a board game where the goal isn’t healing-it’s delaying. The real question isn’t whether patents should exist, but whether we’ve lost the moral compass that says: people shouldn’t die because a corporation filed a patent on a blue pill instead of a red one.
Marie-Pierre Gonzalez
January 6, 2026 AT 02:36 AM
As someone who grew up in Quebec, where generics hit shelves within months of approval, I’m heartbroken. Here, the system is rigged. I’ve seen my friends choose between insulin and rent. This isn’t capitalism-it’s cruelty disguised as law. 🇨🇦❤️🇺🇸
Paige Shipe
January 7, 2026 AT 10:38 AM
Everyone’s so focused on the patents, but nobody talks about the fact that the FDA’s Orange Book is a mess. Companies list patents that don’t even cover the drug’s active ingredient. And the agency just sits there like a librarian with no authority to throw out bad books. Fix the Orange Book first. Then we can talk about caps.
Tamar Dunlop
January 8, 2026 AT 22:05 PM
My heart goes out to every patient forced to ration medication. This isn’t just policy-it’s human suffering. I’ve worked with families who sell their cars to pay for prescriptions. The fact that we tolerate this in a country with the resources to fix it… it’s a moral failure on a national scale. We need courage, not committee reports. The time for silence is over.






Emma Duquemin
December 30, 2025 AT 04:23 AM
This is absolute madness. I had to ration my Eliquis last year because the generic was approved but locked in court for another 18 months. My pharmacist looked at me like I was crazy when I asked why we couldn’t just sell the damn thing. It’s not about innovation-it’s about profit. These companies are treating patients like ATMs with heartbeat monitors. 🤬