Blood clots form when blood thickens and sticks together inside a blood vessel, blocking normal circulation and causing urgent problems.
Deep vein thrombosis, often in the leg, and pulmonary embolism are two dangerous clot types people should know right now. Risk rises after surgery, long travel, pregnancy, cancer, and some birth control methods or genetic clotting problems such as genetics. Common signs include swelling, pain, warmth, redness in a limb, sudden breathlessness, chest pain, or lightheadedness that require urgent care. If you suspect a clot, call emergency services or get to a clinic immediately for proper testing and care now.
Doctors use ultrasound for limb clots, D-dimer blood tests to check clot activity, and CT scans for lung clots too. Most clots are treated with blood thinners like heparin or warfarin and newer direct oral anticoagulants such as apixaban today. These medicines reduce clot growth and lower the risk of dangerous embolism but require monitoring for bleeding signs with guidance. Avoid smoking, stay active, maintain healthy weight, and follow your doctor's advice after surgery to reduce clot risk every day.
Tell your health provider about family clot history, hormone therapy use, or recent injury before prescribing preventive treatment and testing. Some medicines and supplements can increase bleeding risk while on anticoagulants, so share all products you use with clinicians always. If you have cancer, recent major surgery, or long bed rest, discuss prevention options with your team and plan ahead. Pregnant people need special care because clots and treatment choices affect both mother and fetus in different ways ask specialists.
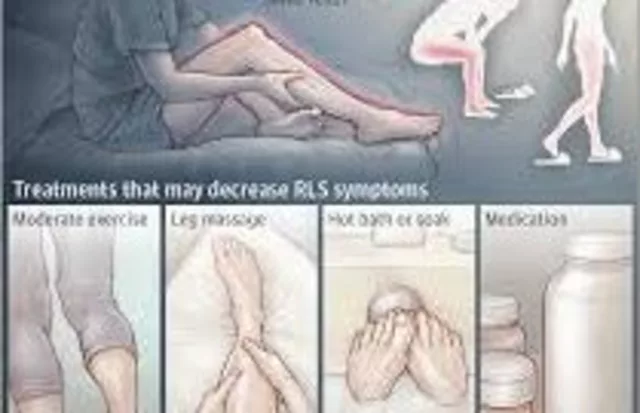
Wear compression stockings after some surgeries or during long travel when your clinician recommends them for clot prevention most times. Know emergency signs: sudden shortness of breath, chest pain that worsens with breath, coughing blood, or fainting get help now. After a clot, follow up matters: stick to blood thinner schedule and attend monitoring appointments regularly to check risk. Lifestyle changes like regular walking, hydration, weight control, and quitting smoking lower long term clot risk effectively over the years.
If you take hormone pills or IVF drugs, ask about clot risks and prevention before starting them consult your doctor. Emergency departments and clot clinics can start treatment fast, which often prevents worse damage and saves lives very quickly now. Know your medications: anticoagulants interact with other drugs, herbs, and foods like grapefruit sometimes increasing bleeding chance ask your clinician. If you miss doses of blood thinners, call the clinic for clear instructions rather than guessing what to do today.
Some people need filters placed in a large vein when anticoagulants are unsafe or ineffective for preventing pulmonary embolism surgically. Questions about surgery timing, travel plans, or medication changes deserve early discussion with your surgeon and prescribing doctor today please. Use credible sources and ask for clear written instructions if you feel unsure about diagnosis or follow up steps now. Understanding clot basics helps you act fast, reduce harm, and talk confidently with your healthcare team about next steps often.

Effective Ways to Prevent Blood Clots After Anesthesia
Blood clots can be a serious risk during recovery from anesthesia and surgery. Understanding prevention strategies and ways to reduce this risk is crucial for a safe and smooth healing process. This article covers practical tips and insights to help you stay informed and proactive. Whether through physical activity, dietary choices, or medical interventions, there are various approaches to consider. Taking control of your postoperative health can make a significant difference in recovery outcomes.
View More