Diabetes treatment: practical steps that work
Diabetes treatment isn't one-size-fits-all. You can control blood sugar with smart daily choices, the right meds, and simple monitoring. This page gives clear steps you can use now, whether you have type 1, type 2, or prediabetes.
First, track your numbers. Use a glucose meter or a continuous glucose monitor and record fasting and post-meal readings for two weeks. Patterns matter more than single numbers: notice what foods, activity, or stress spikes your glucose. Take those notes to your clinician so they can adjust treatment wisely.
Diet and activity that help
Cutting added sugar helps, but focus on consistent carbs and portion size. Pick whole grains, vegetables, and lean proteins. Try a simple rule: halve your plate with vegetables, a quarter with protein, and a quarter with carbs. Walk after meals for 15 to 30 minutes — that lowers post-meal glucose reliably.
Weight loss of 5 to 10% often improves blood sugar for people with type 2 diabetes. You don't need to aim for perfect — steady, realistic changes beat crash diets. If weight loss is tough, ask about structured programs or referral to a dietitian.
Medications and common options
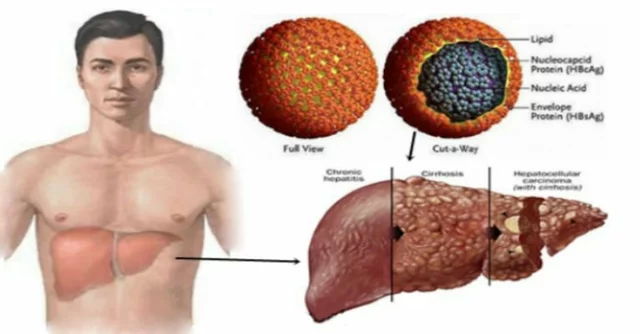
Metformin is usually the first pill for type 2 diabetes because it lowers glucose with low risk of low blood sugar. If metformin isn't enough, newer drugs like SGLT2 inhibitors and GLP-1 receptor agonists add benefits: they lower glucose and can protect the heart and kidneys. Insulin remains essential for type 1 diabetes and often becomes necessary in advanced type 2. Your provider will balance effectiveness with side effects, cost, and routines that fit your life.
Know the warning signs of low blood sugar: sweating, shaking, confusion. Carry fast carbs like glucose tablets. For people on insulin or sulfonylureas, have a plan for hypoglycemia and teach friends or family how to help.
Regular checkups matter. Aim for A1c testing every three months when changing therapy, then every six months once stable. Also get annual eye exams, foot checks, and kidney tests (urine albumin and eGFR). Early detection catches problems before they get serious.
Technology can simplify care. Continuous glucose monitors and connected insulin pens or pumps reduce guesswork. Even simple apps that log food and activity help you spot trends. If tech feels overwhelming, start small: a meter and a notebook work fine.
Mental health affects diabetes control. Stress and depression can raise glucose and make self-care harder. Talk to your clinician about counseling, support groups, or medications if mood is interfering with treatment.
Lastly, ask questions. What A1c goal should you target? Could a newer medication help your heart or kidneys? How can your routine fit work or family life? Good diabetes care is a team effort between you and your healthcare providers.
Start small and be consistent. Wins stack up: cut one sugary drink, walk ten minutes daily, test more often. Track progress and celebrate changes. If something doesn't work, try another approach with your care team until you find what sticks.

Top 7 Alternatives to Glipizide You Should Know About
Tired of the same old diabetes meds? Glipizide's not the only game in town. Let's chat about some top-notch alternatives that could better suit your needs. We'll cover all the pros and cons to help you make the best choice for managing blood sugar levels.
View More