
When a medication triggers anaphylaxis, seconds matter. It’s not a slow, predictable reaction-it hits fast, and it can kill in minutes. You don’t need to be a doctor to save a life. You just need to know what to do, and do it without hesitation.
What anaphylaxis from medication really looks like
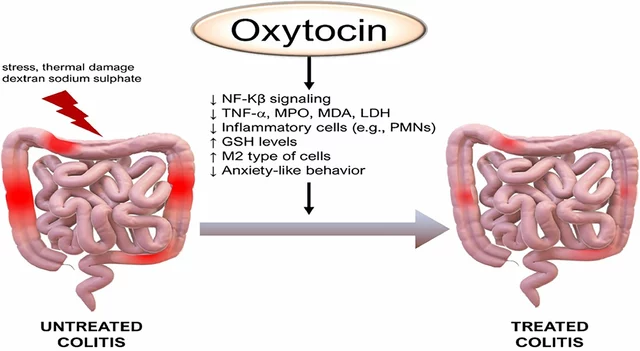
Anaphylaxis isn’t just a rash or a stuffy nose. It’s a full-body emergency where your airway, breathing, and circulation start shutting down. Medications like penicillin, NSAIDs (think ibuprofen or naproxen), chemotherapy drugs, contrast dyes used in scans, and muscle relaxants during surgery are the most common triggers. In hospitals, about 1 in every 2,000 to 5,000 doses causes a reaction. Outside the hospital, it’s rarer-but no less dangerous. What makes it so deadly? Unlike typical allergies, anaphylaxis doesn’t always start with hives or itching. In fact, 10 to 20% of cases show no skin symptoms at all. That’s why people delay action-they think, “It’s not that bad.” But if someone suddenly struggles to breathe, their voice turns hoarse, their tongue swells, or they feel dizzy and pale, it’s already too late to wait.The one thing that saves lives: epinephrine
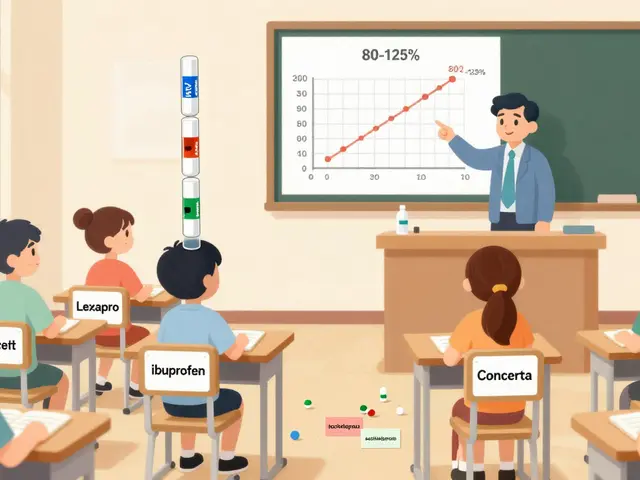
There is no substitute. No antihistamine, no steroid, no home remedy. Only epinephrine can reverse the life-threatening effects of anaphylaxis. It tightens blood vessels, opens airways, and supports heart function-all in under five minutes. The correct dose is given by injecting into the outer thigh muscle. For adults and children over 30 kg, that’s 0.3 mg. For kids between 15 and 30 kg, it’s 0.15 mg. Auto-injectors like EpiPen, Auvi-Q, or Adrenaclick are designed to make this simple. You don’t need to remove clothing-just press firmly against the thigh until you hear a click. Hold it there for 10 seconds. Then remove it. Why not wait to see if it gets worse? Because it won’t. It’ll get worse faster. Studies show that in 70% of fatal cases, epinephrine was never given-or was given too late. The Resuscitation Council UK says: “If in doubt, give adrenaline.” That’s not a suggestion. It’s the law of survival.What to do immediately after giving epinephrine
Giving the shot is only half the battle. The next steps are just as critical.- Lay the person flat. No sitting up. No standing. Even if they’re struggling to breathe, lying flat keeps blood flowing to the heart and brain. If they’re vomiting or unconscious, roll them onto their left side-especially if they’re pregnant.
- Call emergency services immediately. Dial 911 in the U.S., 000 in Australia, or 111 in New Zealand. Don’t wait. Don’t text. Call. Epinephrine wears off in 10 to 20 minutes. Symptoms can come back harder. That’s called a biphasic reaction, and it happens in up to 20% of cases. They need to go to the hospital.
- Give a second dose if needed. If symptoms don’t improve-or get worse-after 5 minutes, give another injection. Same spot. Same technique. Some guidelines say you can repeat every 5 to 10 minutes until help arrives.

What NOT to do
There are myths about anaphylaxis that get people killed.- Don’t give antihistamines like Benadryl first. They help with itching and hives, but they do nothing for breathing or blood pressure. Using them instead of epinephrine delays treatment. In one study, patients given antihistamines alone had no better survival rate than those given nothing.
- Don’t give steroids unless instructed by a doctor. Corticosteroids like hydrocortisone were once routine, but current guidelines say they don’t stop the immediate danger. They may help prevent a delayed reaction, but they’re not emergency treatment.
- Don’t let them walk or stand. Standing during anaphylaxis causes blood to pool in the legs. Blood pressure crashes. Death follows within seconds. This has been shown in simulations and real cases. Lying flat isn’t optional-it’s mandatory.
Why people delay-and how to beat it
In hospitals, the average time to give epinephrine after symptoms appear is over 8 minutes. That’s too late. Why? Nurses and doctors often hesitate because they’re afraid of side effects-racing heart, high blood pressure. But here’s the truth: out of 35,000 epinephrine doses given for anaphylaxis, only 0.03% caused serious heart problems. The risk of not giving it? Up to 10% death rate. Outside hospitals, patients themselves delay. A 2023 survey found that 68% of people with known allergies carry an auto-injector, but only 41% feel confident using it. Many don’t know how to hold it long enough. Others inject into fat instead of muscle. Some think, “I’ll just wait and see.” Practice matters. Take 2 minutes today. Watch a video of how to use an EpiPen. Hold a trainer pen (they’re free from pharmacies) and simulate the injection. Do it on a pillow. Do it with your eyes closed. Make it automatic.Special cases: what changes when the person is on other meds
If someone is taking beta-blockers (common for high blood pressure or heart conditions), epinephrine may not work as well. Their body blocks the drug’s effect. In these cases, higher doses may be needed-sometimes two or three times the usual amount. They’re also more likely to have severe, prolonged reactions. Pregnant women need special positioning. Lying flat on the back can squish the main blood vessel supplying the baby. Always roll them onto their left side. Keep them flat. Don’t let them sit up. Children are different too. Don’t hold them upright. Keep them flat. Even if they’re crying or scared, lying down keeps their circulation stable.After the emergency: what happens next
Even if they seem fine after the first shot, they must go to the hospital. Biphasic reactions can hit 1 to 72 hours later. That’s why guidelines say: minimum 4 hours of observation. For medication-induced cases, recent data suggests 6 to 8 hours may be safer. At the hospital, they’ll get IV fluids to support blood pressure, oxygen if needed, and possibly more epinephrine if symptoms return. They’ll be monitored for heart rhythm changes and breathing problems. Afterward, they need an allergy referral. The goal isn’t just to survive this episode-it’s to prevent the next one. They’ll need to carry two epinephrine auto-injectors at all times. They’ll need to learn how to recognize early signs. And they’ll need a written action plan.What’s new in 2025
The FDA approved a new auto-injector with voice guidance in 2023. It tells you step-by-step what to do. In trials, untrained users got it right 89% of the time-up from 63%. That’s huge. New research is also looking at dosing based on body mass index (BMI), not just weight. Obese patients often get underdosed because standard pens don’t deliver enough into deep muscle. Early results show better outcomes when dosing is adjusted. And in 2025, updated guidelines are expected to recommend longer observation for medication-triggered cases-because they’re more likely to come back.Final reminder: act fast, act sure
Anaphylaxis from medication doesn’t ask for permission. It doesn’t wait for you to check your phone or call a doctor. It acts. And so must you. If someone has trouble breathing, swelling in the throat, dizziness, or sudden collapse after taking a drug-epinephrine now is the only rule that matters. No delay. No doubt. No exceptions. You don’t need to be brave. You just need to be ready.12 Comments
Debbie Naquin
December 3, 2025 AT 14:14 PM
The epinephrine paradox is that its physiological effects-alpha-1 agonism, beta-1 inotropy, beta-2 bronchodilation-are precisely what counteract the cytokine storm and vasodilatory shock of anaphylaxis. Yet we treat it like a last resort instead of the first-line neurochemical intervention it is.
Karandeep Singh
December 4, 2025 AT 08:35 AM
epinephrine is overrated tbh. i had a reaction once and drank lemon water. fine.
elizabeth muzichuk
December 5, 2025 AT 12:08 PM
Someone just drank lemon water? Are you serious? You’re not just risking your own life-you’re making the rest of us look like idiots who actually take this seriously. This isn’t a TikTok trend, it’s a medical emergency. If you don’t know how to use an EpiPen, you shouldn’t be allowed near a pharmacy.
Mary Ngo
December 5, 2025 AT 20:30 PM
Have you considered that the entire medical-industrial complex has weaponized fear of anaphylaxis to sell auto-injectors? The 10% mortality rate? Fabricated. The biphasic reaction? Overstated. The real danger is the normalization of pharmaceutical dependency. They want you to carry two pens because they profit from your paranoia.
James Allen
December 7, 2025 AT 16:22 PM
Wow, so now we’re supposed to trust some fancy FDA-approved gadget just because it talks to you? In America, we used to be tough. We didn’t need voice-guided pens-we had grit. I’d rather just stab it in with my teeth if I had to. That’s real American courage.
Scotia Corley
December 8, 2025 AT 13:35 PM
It is not merely advisable, but ethically imperative, to administer epinephrine without hesitation upon recognition of any systemic symptomatology indicative of anaphylaxis. Delay constitutes negligence, regardless of intent or circumstance.
amit kuamr
December 8, 2025 AT 14:10 PM
epinephrine is just a bandaid. real solution is avoiding meds entirely. why do we even use these drugs? pharma owns everything. you think you're safe with your pen but they're still watching
Rachel Stanton
December 9, 2025 AT 00:58 AM
For anyone new to this-don’t overthink it. The thigh is the target. Press. Hold 10 seconds. That’s it. No need to remove jeans. No need to wait. If you’re unsure, you’re already late. Practice with a trainer pen. Keep it next to your keys. Make it automatic. You’re not a hero-you’re just prepared.
Amber-Lynn Quinata
December 9, 2025 AT 09:57 AM
OMG I JUST REALIZED I NEVER CHECKED MY EPI PEN EXPIRATION DATE 😱 I HAVE TWO BUT ONE IS FROM 2021 😭 I’M GOING TO THE PHARMACY RIGHT NOW 🏃♀️💨 #epipenlife #anaphylaxisawareness
Charlotte Collins
December 10, 2025 AT 16:16 PM
They say epinephrine is the only thing that works. But have you ever seen the side effects? The tremors, the panic, the heart pounding like it’s trying to escape? It’s not a cure-it’s a chemical sledgehammer. And they call it saving lives? What about the psychological trauma of being injected by strangers while you’re choking? Nobody talks about that.
ariel nicholas
December 10, 2025 AT 16:24 PM
Wait-so you’re telling me that in 2025, we’re going to adjust dosing based on BMI? But we’ve been using the same weight-based guidelines since the 80s? And now you want to change it because someone’s fat? That’s not science-that’s social engineering. If you’re obese, maybe you shouldn’t be taking meds in the first place. Just sayin’.


Erin Nemo
December 2, 2025 AT 14:45 PM
Just carried my EpiPen for 3 years and never used it. Today I watched a 10-second video on how to use it. Done. No more fear.