LGBTQ Health Care: Essential Information and Resources
When talking about LGBTQ health care, the medical services that respect and address the unique needs of lesbian, gay, bisexual, transgender, and queer patients. Also known as LGBTQ medical care, it spans everything from routine check‑ups to specialized hormone regimens.
One core pillar is gender-affirming hormone therapy, a set of medications used to align a person’s physical traits with their gender identity. This therapy directly influences mental well‑being, bone health, and cardiovascular risk, so clinicians need to monitor labs, adjust doses, and counsel on side effects. Another crucial area is STI prevention, screening, vaccination, and prophylactic measures that lower rates of HIV, HPV, and other infections in LGBTQ communities. Effective prevention lowers long‑term complications and supports healthier relationships. Finally, inclusive primary care, a welcoming environment where providers ask the right questions and respect pronouns creates the foundation for all other services.
Why These Areas Matter Together
LGBTQ health care encompasses gender‑affirming hormone therapy, STI prevention, mental health support, and inclusive primary care. When a clinic offers hormone monitoring, it also needs routine STI testing because hormone changes can affect immune response. STI prevention influences LGBTQ health outcomes by reducing infection‑related fatigue, a topic you’ll see in articles about urinary tract infections and chronic fatigue. Mental health support ties back to hormone therapy, as fluctuations in estrogen or testosterone can trigger mood shifts that require counseling or medication adjustments.
Practical steps start with finding a provider who understands these intersections. Look for clinics that list hormone therapy expertise, have clear STI screening protocols, and advertise staff training on LGBTQ cultural competence. Ask about the lab schedule for hormone levels, the frequency of Pap smears or HPV testing for trans men, and whether they can prescribe PrEP or post‑exposure prophylaxis. Your provider should also discuss lifestyle factors—like alcohol’s impact on bladder control—that matter for both hormone stability and infection risk.
Medication safety is a recurring theme in our article collection. For example, antibiotics like clindamycin or cefuroxime may be prescribed after a urinary infection, but they can interact with hormone blockers or affect gut flora, which in turn influences hormone metabolism. Antivert (meclizine) for motion sickness is another drug that, while not directly related to gender care, illustrates how side‑effect profiles differ across patients with varying hormone levels. Understanding these nuances helps you ask the right questions and avoid unexpected side effects.
Beyond prescriptions, self‑care habits play a big role. Staying hydrated reduces gout attacks—a concern for patients on certain diuretics—and can also lessen urinary urgency that some trans women experience with estrogen therapy. Nutrition advice for alopecia, kidney disease itching, and severe stomach pain shows how systemic health ties back to the core of LGBTQ health care. When you combine medical guidance with everyday habits, you build a resilient foundation for long‑term wellness.
What you’ll discover in the posts below is a mix of drug comparisons, safety tips, and condition‑specific guidance that all feed into a holistic LGBTQ health strategy. From buying affordable generic Allegra for allergy relief to navigating the side‑effects of antidepressants, each article adds a piece to the puzzle of comprehensive care. Keep reading to find actionable insights, evidence‑based recommendations, and practical tools that empower you to manage your health with confidence.
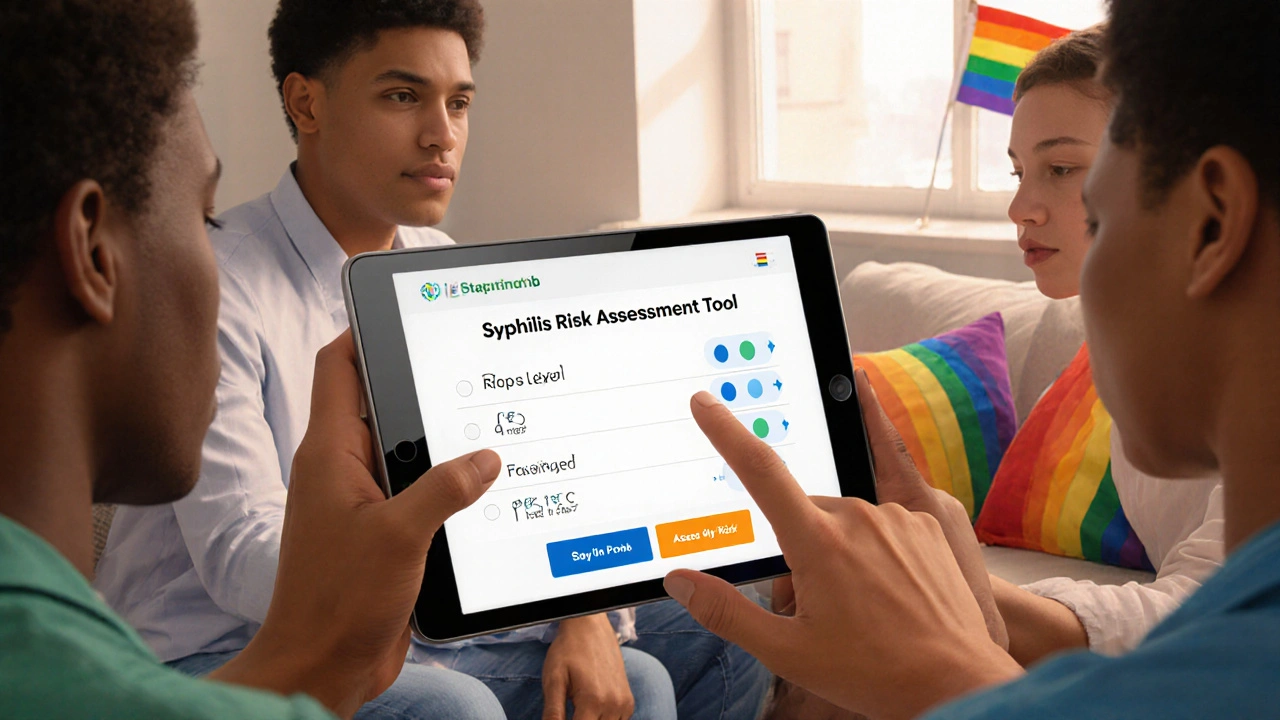
Syphilis in the LGBTQ+ Community: Addressing Disparities and Barriers to Care
Explore why syphilis rates are higher in the LGBTQ+ community, the barriers to care, and practical steps and resources to close the gap.
View More