Nodular Acne: what it is and what really helps
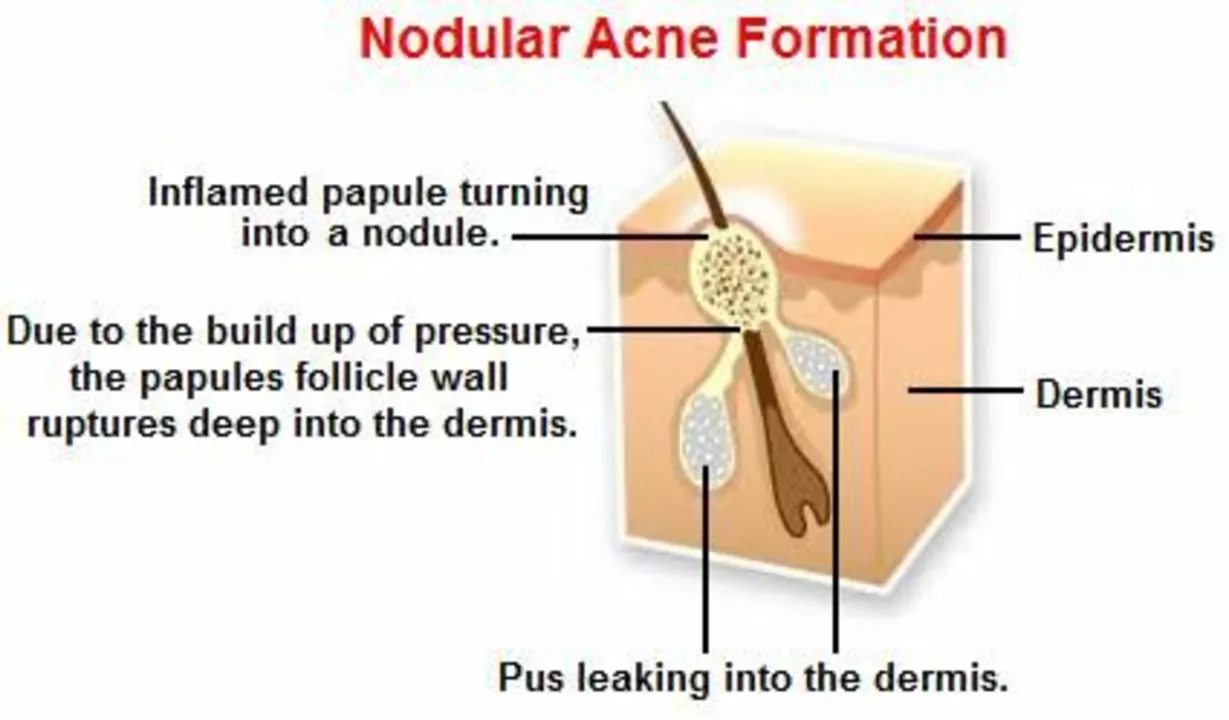
Nodular acne shows up as hard, deep, painful lumps under the skin. These are not the small whiteheads you can pop. Nodules form deep in the skin and can last weeks or months. They also raise the risk of permanent scars, so acting early matters.
What causes nodular acne?
Three things usually team up: blocked pores, excess oil, and bacteria. But nodules form when inflammation goes deeper and stronger than with regular pimples. Hormonal swings (teen years, menstrual cycles), genetics, certain medicines, and picking at spots can all make nodular acne more likely. Stress and sweat won’t cause it alone, but they can make flare-ups worse.
How to treat nodular acne — what works now
Want quick relief while avoiding scars? Start with safe home care and move to medical options if needed.
Home care: apply warm compresses for 10–15 minutes a few times a day to ease pain and help inflammation settle. Don’t squeeze or pick — that makes scarring much more likely. Use a gentle, non-drying cleanser twice daily and avoid heavy oils or greasy makeup.
Over-the-counter help: benzoyl peroxide can reduce surface bacteria and inflammation. Topical retinoids (adapalene) help unclog pores but take weeks to work and may irritate at first.
When lesions are large, painful, or lasting weeks, see a dermatologist. Medical treatments that actually stop nodules include:
- Intralesional steroid injection: a dermatologist injects a tiny steroid into a nodule to shrink it fast and reduce pain. This often works within days and lowers scarring risk when done correctly.
- Oral antibiotics: short courses reduce inflammation and bacterial load. They’re not a long-term fix and should be paired with topical treatments to prevent resistance.
- Hormonal therapy: for people assigned female at birth, birth control pills or spironolactone can control hormonal acne that causes nodules.
- Isotretinoin: this oral medication can clear even severe nodular acne long-term. It needs close medical monitoring because of side effects and pregnancy risks.
Minor procedures: for very large, fluid-filled cysts a dermatologist may drain them, but routine lancing of nodules is not recommended at home.
When to see a doctor now: if nodules are painful, multiply quickly, bleed, or leave dents in the skin, make an appointment. Also see a doctor if OTC care hasn’t helped after 6–8 weeks.
Preventing scars: early treatment is the best prevention. Use sunscreen daily (scars and post-inflammatory marks darken in sun). After active acne clears, talk to your dermatologist about laser, microneedling, or chemical peels to improve texture.
Dealing with nodular acne can feel overwhelming, but effective options exist. If you have painful or stubborn nodules, book a dermatologist consult — fast action saves skin.
The Role of Hydration in Nodular Acne Prevention and Management
As a blogger, I've discovered the crucial role hydration plays in preventing and managing nodular acne. Keeping our body well-hydrated helps flush out toxins, maintain healthy skin, and reduce inflammation. Drinking enough water daily can significantly improve our skin's overall appearance and texture. Incorporating hydrating skincare products, like hyaluronic acid, also aids in maintaining our skin's moisture levels. So, let's prioritize staying hydrated for clearer and healthier skin!
View More