
When you live with Borderline Personality Disorder (BPD), emotions don’t just come and go-they crash over you like a wave with no shore. One moment you’re fine, the next you’re drowning in shame, rage, or emptiness. And when that happens, the urge to hurt yourself, push people away, or disappear can feel overwhelming. That’s not weakness. It’s a neurological and emotional response shaped by years of invalidation, trauma, or unstable relationships. But here’s the truth: DBT skills can change that. Not by fixing who you are, but by giving you tools to survive the storm without self-destruction.
What DBT Actually Does for BPD
Dialectical Behavior Therapy, or DBT, wasn’t created to cure Borderline Personality Disorder. It was built to help people live with it-without dying from it. Developed by Dr. Marsha Linehan in the late 1980s, DBT came out of frustration. Standard talk therapy wasn’t working for people who were chronically suicidal or self-harming. They needed more than insight. They needed survival skills. DBT works because it doesn’t fight your emotions. It teaches you how to hold them without letting them control you. It’s not about being calm all the time. It’s about knowing what to do when you’re not calm. The therapy combines acceptance (you’re allowed to feel this way) with change (here’s how to move through it). And it’s backed by science. A 2006 study showed people using DBT reduced self-harm by 46% compared to those getting regular care. That’s not a small win. That’s life-saving.The Four Core Skill Modules
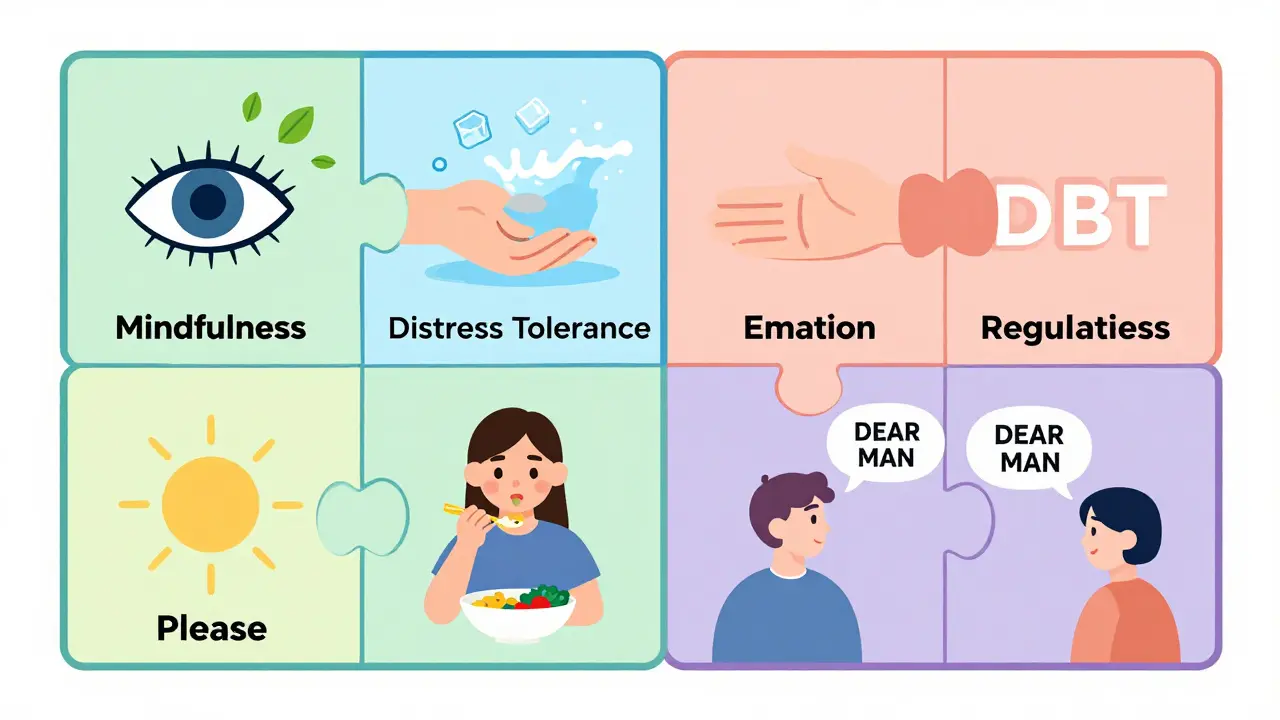
DBT isn’t one skill. It’s four sets of skills, each targeting a different part of the BPD experience. You don’t need to master them all at once. Start with one. Build from there.- Mindfulness: This is your anchor. It’s not meditation in the spiritual sense. It’s learning to notice what’s happening inside you-without judging it. You practice observing your thoughts, feelings, and urges without reacting. Simple? No. Easy? Not at first. But after eight weeks, people with BPD show a 32% improvement in emotional regulation. That’s because mindfulness creates space between the trigger and the reaction.
- Distress Tolerance: This is your crisis toolkit. When everything feels like it’s falling apart, this module gives you immediate strategies. TIPP (Temperature, Intense exercise, Paced breathing, Paired muscle relaxation) works fast. Splash cold water on your face. Do 20 jumping jacks. Breathe in for five seconds, out for six. These tricks don’t fix the problem-but they stop you from making it worse. Studies show people using these techniques cut ER visits for self-harm by 57% in the first four months.
- Emotion Regulation: This is where you learn why your emotions are so intense-and how to calm them down. PLEASE (Treat Physical Illness, Balanced Eating, Avoid mood-altering drugs, Balanced Sleep, Exercise) sounds basic, but it’s powerful. If you’re sleep-deprived or skipping meals, your brain can’t regulate emotion. One study found consistent use of this module reduced emotional reactivity by 40% in six months. Then there’s Opposite Action: if you feel like screaming at someone, you practice speaking softly instead. It sounds fake, but your brain learns from behavior, not intention.
- Interpersonal Effectiveness: You’re not alone, but you might feel like it. This module teaches you how to ask for what you need without losing the relationship. DEAR MAN (Describe, Express, Assert, Reinforce, stay Mindful, Appear confident, Negotiate) helps you say, “I’m feeling abandoned when you cancel plans. I need us to reschedule. Can we do that?” GIVE (be Gentle, show Interest, Validate, use Easy manner) helps you repair damage after an argument. FAST (be Fair, no Apologies, Stick to values, be Truthful) keeps you from sacrificing your worth to keep peace.
Crisis Planning: Your Personal Survival Guide
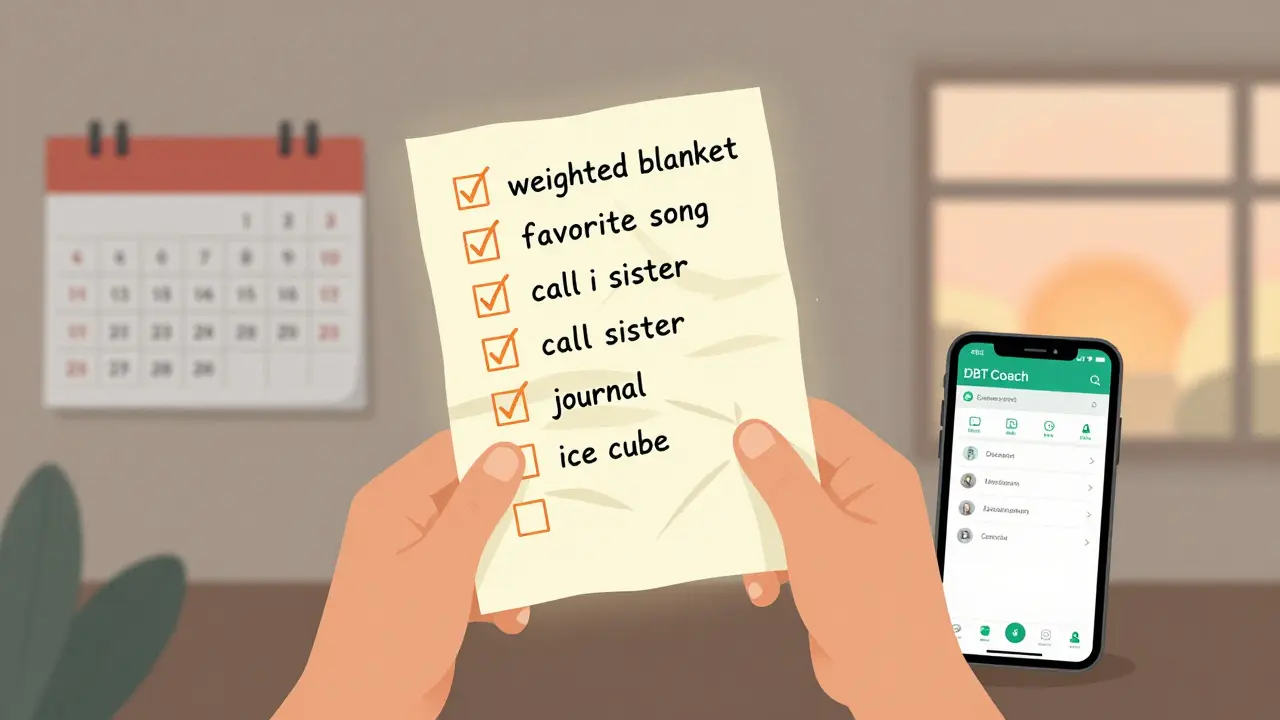
A crisis isn’t always a suicide attempt. Sometimes it’s sitting on the bathroom floor at 3 a.m., shaking, unable to breathe, convinced you’re worthless. That’s when you need a plan-not a pep talk. DBT crisis planning starts with STOP: Stop (don’t act), Take a step back (breathe), Observe (what’s happening in your body? What thoughts are looping?), Proceed mindfully (pick one skill from your toolkit). You write this down. You keep it on your phone. You put it on your fridge. You also build a personalized list of things that help. Maybe it’s listening to a specific song. Walking around the block. Calling your sister. Holding a weighted blanket. Writing in a journal. You don’t wait until you’re in crisis to figure this out. You build it while you’re stable. And you update it every month. One user on Reddit said: “I used IMPROVE-Imagery, Meaning, Prayer, Relaxation, One thing in the moment, Vacation, Encouragement-to get through the night without self-harming for the first time in 10 years.” That’s not magic. That’s planning.How DBT Compares to Other Treatments
You might have heard of other therapies for BPD: Mentalization-Based Therapy (MBT), Schema Therapy, Transference-Focused Psychotherapy (TFP). Here’s how DBT stacks up:| Treatment | Reduction in Self-Harm | Time Commitment | Best For |
|---|---|---|---|
| DBT | 35-46% | 6-12 months, 2-3 hours/week | Chronic suicidality, emotional flooding, self-harm |
| Mentalization-Based Therapy (MBT) | 22% | 18 months, weekly sessions | Understanding others’ intentions, attachment issues |
| Schema-Focused Therapy | 28% | 12-18 months, weekly sessions | Deep-seated beliefs about self-worth |
| Transference-Focused Psychotherapy (TFP) | 25% | Weekly 50-minute sessions | Identity disturbance, less acute crisis |
| STEPPS (group-based) | 30% | 20 weeks | People who can’t commit to individual therapy |
What It Really Takes to Make DBT Work
DBT isn’t a quick fix. It’s a lifestyle shift. You’ll need:- Weekly individual therapy (1 hour)
- Weekly group skills training (2 hours)
- 24/7 phone coaching access
- Homework. Yes, homework. Worksheets, logs, skill trackers.
Accessing DBT: Is It Available to You?
There are only about 1,842 certified DBT therapists worldwide. In rural areas, access is still a problem. Only 12% of rural U.S. communities have one. But telehealth has changed that. Since 2020, access has increased by 28%. Many insurers now cover 12-20 sessions a year. Medicare and most private plans include DBT if it’s delivered through a certified program. You can also use apps like DBT Coach or Virtual Reality DBT. A 2023 study found people using these tools stuck with treatment 68% of the time-compared to 45% with paper worksheets. They’re not replacements, but they help.Real People, Real Results
Reddit’s r/BPD and r/DBT communities are full of stories like this:- “I was about to leave my partner during an argument. Instead, I used DEAR MAN. I said, ‘I feel scared when you don’t reply. I need to know you’re still here.’ He stayed. We talked. I didn’t burn the bridge.”
- “I used TIPP during a panic attack. I ran in place for 90 seconds, then held ice cubes. My heart slowed. I didn’t cut. That was the first time in years.”
- “My therapist never told me I was ‘too sensitive.’ She said, ‘Your emotions are loud, but they’re valid. Now let’s learn how to carry them.’ That changed everything.”
What Doesn’t Work
DBT isn’t magic. It won’t erase your past. It won’t make your family understand. It won’t stop you from feeling pain. Some experts, like Dr. Joel Paris, argue it focuses too much on behavior and not enough on deep personality change. And yes-some people still struggle with identity issues even after years of DBT. But if your goal is to stop self-harming, to not lose your relationships, to survive the night without breaking-you don’t need a cure. You need tools. And DBT gives you more than any other treatment.Where to Start
If you’re reading this and thinking, “I need this,” here’s your first step:- Find a DBT-certified therapist. Check the Linehan Institute’s directory or ask your current provider.
- Ask if they offer a skills group. You need both individual and group therapy.
- Get the DBT Skills Training Manual (Second Edition) or The Dialectical Behavior Therapy Skills Workbook. Read one section. Don’t try to do it all.
- Write down your crisis plan. What helps when you’re falling apart? List five things. Put them where you’ll see them.
- Start with one skill. Mindfulness. TIPP. PLEASE. Pick one. Practice it for two weeks. No pressure. Just try.
Can DBT help someone who doesn’t self-harm but has intense emotional swings?
Yes. While DBT was originally designed for people with self-harm behaviors, its skills are effective for anyone struggling with emotional dysregulation. The Emotion Regulation and Distress Tolerance modules help people manage anger, anxiety, and mood swings-even without suicidal thoughts. Many people use DBT to improve relationships, reduce impulsivity, and handle workplace stress.
How long until I see results from DBT?
Most people notice small changes within 2-4 months. Reduced frequency of outbursts, better sleep, fewer arguments. Major shifts-like stopping self-harm or holding onto relationships-usually take 6-12 months. The key is consistency, not perfection. Even practicing one skill once a week builds momentum.
Is DBT only for women?
No. While early research focused on women with BPD, DBT has been successfully adapted for men, teens, and non-binary individuals. Men often respond even better to the structured, skills-based approach because it gives them clear actions instead of vague emotional exploration. DBT is gender-neutral in practice.
Can I do DBT on my own without a therapist?
You can learn the skills from books or apps, but full DBT requires professional guidance. The phone coaching, group feedback, and therapist support are what make it effective. Trying to do it alone is like trying to learn to swim without ever getting in the water. Use workbooks as a supplement-not a replacement.
What if I can’t afford DBT?
Many community mental health centers offer low-cost or sliding-scale DBT programs. University clinics often train therapists who provide services at reduced rates. Online groups like DBT Peer Support on Facebook are free and offer accountability. Some apps, like DBT Coach, have free versions. Don’t wait for perfect conditions. Start with what you have.
Do DBT skills work during a full-blown crisis?
They can, if you’ve practiced them when you were calm. During extreme distress, your brain can’t access complex thoughts. That’s why skills like TIPP and STOP are designed to be simple, physical, and automatic. You don’t think your way through a crisis-you act your way through it. Practice when you’re okay so you can use it when you’re not.
Is DBT the only treatment for BPD?
No. Other therapies like MBT and Schema Therapy are also evidence-based. But DBT is the only one with strong, consistent results for reducing self-harm and suicide attempts. It’s the gold standard for crisis management. If your main goal is survival and stability, DBT is your best starting point.
Final Thought
You’re not broken. You’re not too much. You’re not a burden. You’re someone who learned early on that the world doesn’t hold space for your pain-and now you’re learning how to hold it yourself. That’s not easy. But it’s possible. And you don’t have to do it alone.17 Comments
Chuck Dickson
January 19, 2026 AT 19:52 PM
Hey-just wanted to say this post gave me chills. Not because it’s perfect, but because it’s real. I’ve been in DBT for 14 months now, and I still forget to use my skills until I’m knee-deep in panic. But now? I have a sticky note on my mirror that says ‘Breathe first, react later.’ I didn’t think I’d ever say this, but… I’m alive because of this stuff.
It’s not magic. It’s not easy. But it’s worth showing up for-even on the days you feel like a failure. You’re not broken. You’re learning. And that’s enough.
One day at a time. One skill at a time. You’ve got this.
Dayanara Villafuerte
January 19, 2026 AT 20:19 PM
OMG YES 🙌 I used the IMPROVE technique last week when my ex ghosted me AGAIN. Imagery: I pictured myself as a sturdy oak tree. Meaning: I’m not defined by his actions. Prayer: I whispered ‘I am safe’ 17 times. Relaxation: I lit a candle and stared at the flame like a weirdo. One thing: I just focused on the smell of lavender. Vacation: I took a 20-minute nap. Encouragement: I texted myself ‘You’re doing better than you think.’
Didn’t cry. Didn’t text him back. Didn’t delete my Instagram. 🎉
DBT isn’t glamorous. But it’s the only thing that didn’t make me want to throw my phone out the window. Also, TIPP saved me during a panic attack in Target. I ran in place while pretending I was in a TikTok dance challenge. People stared. I didn’t care. I was alive.
PS: The worksheet on my fridge? It’s covered in coffee stains and glitter. And I love it.
Andrew Qu
January 21, 2026 AT 15:38 PM
For anyone feeling overwhelmed by the idea of starting DBT: pick one thing. Just one. Maybe it’s ‘TIPP’ or ‘PLEASE.’ Do it for 3 days. Don’t aim for perfection. Just show up. The goal isn’t to ‘fix’ yourself-it’s to give yourself a fighting chance.
I used to think I had to be ‘ready’ to heal. Turns out, healing doesn’t wait for readiness. It waits for small, stubborn actions.
You don’t need to be an expert. You just need to be willing to try. And that’s more than enough.
Jay Clarke
January 23, 2026 AT 09:31 AM
Let’s be real-this is just another way for therapists to make money. ‘Oh, you’re in crisis? Here’s a $200/hour worksheet.’ And don’t get me started on the group sessions. I spent 6 months sitting in a circle with 7 other people crying about their childhoods while the therapist took notes like she was writing a novel.
Also, why is everyone acting like DBT is the only thing that works? What about ACT? CBT? Even just getting a dog helped me more than any ‘opposite action’ ever did.
And the ‘crisis plan’? That’s just a fancy way of saying ‘write down what distracts you.’ I used to write ‘watch anime’ and ‘eat ice cream.’ Worked better than breathing exercises.
Also, the ‘phone coaching’? Sounds like a scam. Who’s on the other end? A grad student? A bot? I’d rather call my cousin who says ‘I’m here’ and doesn’t ask me to fill out a form.
And why is this post so long? Did someone get paid per word?
Look-I get that people want to help. But this feels like a cult manual with graphs.
Selina Warren
January 24, 2026 AT 20:27 PM
People act like DBT is a magic pill, but here’s the truth: it’s the only thing that doesn’t tell you you’re broken. Every other therapy says ‘dig into your trauma’ or ‘change your core beliefs.’ DBT says: ‘You’re not broken. You’re overwhelmed. Here’s how to hold it.’
And yes, it’s tedious. Yes, it’s boring. Yes, you’ll hate the worksheets. But when you’re on the floor at 3 a.m. and your brain is screaming ‘you’re worthless,’ you don’t need a lecture-you need a tool. And TIPP? That’s a tool. Not a metaphor. Not a pep talk. A physical, immediate, undeniable intervention.
Also, the fact that men are underrepresented in DBT research doesn’t mean it doesn’t work for them. I’m a guy. I’ve used DEAR MAN to tell my boss I needed a mental health day. He didn’t fire me. He thanked me.
Stop romanticizing suffering. Start practicing survival.
Robert Davis
January 26, 2026 AT 07:02 AM
Interesting. But I’ve read the original Linehan papers. The 46% reduction in self-harm? That’s compared to treatment-as-usual-which often meant ‘no therapy.’ The real comparison should be against other evidence-based therapies, not just ‘whatever the clinic was doing before.’
Also, the ‘phone coaching’ component? That’s the only part that’s actually unique. Everything else? Mindfulness? Distress tolerance? Those are in CBT, ACT, even mindfulness-based stress reduction. DBT just packaged them with a pretty bow and a 12-month curriculum.
And the ‘homework’? That’s the part that makes people drop out. Most people with BPD are already overwhelmed by structure. Adding more structure is like giving a drowning person a spreadsheet.
Don’t get me wrong-I’ve seen people benefit. But let’s stop acting like this is the only path. It’s one path. A good one. But not the only one.
Also, the stats on telehealth? That’s not DBT. That’s an app. Don’t confuse digital tools with therapy.
Eric Gebeke
January 27, 2026 AT 11:09 AM
I’ve been doing DBT for 3 years. I’ve been in and out of hospitals. I’ve tried meds, therapy, ECT, even hypnosis. DBT is the only thing that didn’t make me feel like a lab rat.
But let me tell you what nobody says: it’s not about the skills. It’s about the therapist. If your therapist is cold, dismissive, or just going through the motions? You’ll quit. No matter how good the manual is.
I had one therapist who looked me in the eye and said, ‘I don’t care if you’re ‘too emotional.’ I care that you’re here.’ That’s what changed everything.
Skills are tools. But connection? That’s the cure.
Also, the ‘crisis plan’? Mine says ‘call my sister. If she doesn’t answer, call the crisis line. If they’re busy, scream into a pillow. Then drink water.’ Simple. Human. Real.
Stop making this complicated. Just be kind to yourself.
Jake Moore
January 28, 2026 AT 15:13 PM
For anyone thinking ‘I can’t afford this’-you don’t need a certified DBT therapist to start. Get the workbook. Read one module. Pick one skill. Try it for two weeks. No pressure. No judgment.
I started with ‘opposite action.’ Felt ridiculous. But when I was furious at my roommate and instead of yelling, I made them tea? We talked. We didn’t fight. That was the first time in years I didn’t feel like I was losing control.
It’s not about being perfect. It’s about being present.
You’re not behind. You’re not broken. You’re just learning how to hold yourself.
And that’s enough.
Max Sinclair
January 28, 2026 AT 16:00 PM
This post is thoughtful, well-researched, and deeply human. I appreciate how it avoids the trap of ‘DBT fixes everything’ while still honoring its power. The comparison table is especially helpful-clear, factual, no fluff.
I’ve been in DBT for 2 years. I still struggle. But now I have a language for my pain. I can say, ‘I’m in distress mode’ instead of ‘I’m a disaster.’ That shift? Priceless.
Also, the fact that you mentioned men? Thank you. Too many assume BPD is a ‘woman’s disorder.’ I’m a man. I’ve used DEAR MAN to ask for help at work. It felt terrifying. It worked.
DBT isn’t about becoming someone else. It’s about becoming more of yourself-with less self-destruction.
Thank you for writing this.
Praseetha Pn
January 28, 2026 AT 22:55 PM
DBT? Pfft. In India, we don’t need worksheets to survive. We have chai, family yelling, and Bollywood songs. I cried for 3 hours after my boyfriend left me. Then I danced to ‘Tum Se Hi’ and ate samosas. That’s my TIPP. Cold water? No. Spicy food? YES.
Also, why are you all so obsessed with ‘skills’? In my culture, we don’t ‘regulate emotions’-we let them burn and then move on. You think your ‘opposite action’ is better than my aunt screaming ‘beta, kya hua?’ and then feeding me biryani?
And who made you the boss of mental health? This post reads like a corporate wellness brochure written by someone who’s never been hungry, never been alone, never had to choose between rent and meds.
Also, ‘phone coaching’? In my village, we call our neighbor. They come over. They sit. They don’t charge $150.
Stop Westernizing pain. Not everyone needs a workbook.
Nishant Sonuley
January 29, 2026 AT 09:48 AM
It’s fascinating how Western psychology has turned emotional survival into a structured, modular, time-bound, evidence-based, skill-acquisition paradigm-when in fact, human suffering has always been navigated through ritual, community, storytelling, and the simple, unmediated presence of another human being who doesn’t try to fix you, just sits with you.
DBT, in its clinical form, is a brilliant adaptation for a society that has systematically dismantled those natural supports-families fragmented, communities atomized, elders removed, rituals erased.
So yes, DBT works-not because it’s inherently superior, but because it’s a desperate, beautiful, highly organized attempt to reconstruct what modern life has destroyed.
But let’s not pretend that holding ice cubes is equivalent to being held by someone who loves you.
And let’s not forget: the real ‘skill’ is not in the worksheet-it’s in the courage to keep showing up, even when the system fails you.
So thank you for this post. But let’s also ask: why did we need this in the first place?
Emma #########
January 31, 2026 AT 06:36 AM
I read this after a really bad night. I didn’t cry. I just sat there and thought… maybe I’m not broken. Maybe I’m just learning how to carry weight.
I’ve been doing DBT for a year. I still mess up. I still say things I regret. But now I have a list of five things that help: my cat, the song ‘Hallelujah,’ walking barefoot on grass, writing one sentence in my journal, and calling my sister even if I don’t say anything.
It’s not glamorous. But it’s mine.
Thank you for writing this. I needed to hear it.
Andrew McLarren
January 31, 2026 AT 10:49 AM
While the clinical efficacy of Dialectical Behavior Therapy is well-documented in peer-reviewed literature, the presentation of this material, though well-intentioned, exhibits a degree of rhetorical embellishment that may inadvertently undermine its scientific credibility. The use of emotive language, anecdotal testimonials, and non-peer-reviewed statistics-such as the purported 57% reduction in emergency room visits-risks conflating clinical outcomes with inspirational narrative.
Moreover, the assertion that DBT is the ‘gold standard’ for crisis management, while commonly accepted in certain clinical circles, remains contested in broader psychiatric discourse, particularly regarding long-term personality restructuring.
A more balanced presentation would acknowledge the heterogeneity of treatment responses, the limitations of self-report data in BPD populations, and the critical role of comorbid conditions in moderating therapeutic outcomes.
That said, the structural clarity of the four modules is commendable and provides a useful heuristic for clinicians and patients alike.
Andrew Short
January 31, 2026 AT 20:52 PM
Let’s cut the crap. DBT is just behavioral conditioning for people who can’t handle their feelings. You’re not healing-you’re being trained to perform emotional control like a trained dog.
And who gets to decide what’s ‘healthy’? The same people who told women to ‘calm down’ for centuries.
Also, why is ‘TIPP’ even a thing? You’re supposed to run around like a maniac or hold ice? That’s not therapy-that’s a cult ritual.
And the ‘crisis plan’? That’s just a checklist for people who’ve been told their pain isn’t valid.
Real healing isn’t about skills. It’s about being seen. Being held. Being told it’s okay to be broken.
DBT doesn’t do that. It just gives you tools to hide it better.
And don’t even get me started on the ‘phone coaching.’ That’s not support-that’s a babysitter with a degree.
Chuck Dickson
February 1, 2026 AT 17:53 PM
To the person who said DBT is just training people to perform: I get it. I thought that too. But here’s what changed for me: I used to think I had to be perfect to be loved. Now I know I just have to be present. Even if I’m shaking. Even if I’m crying. Even if I’m holding ice cubes in the bathroom.
DBT didn’t make me quiet. It made me brave enough to be loud without breaking.
And that’s not performance. That’s freedom.
Emma #########
February 3, 2026 AT 17:22 PM
Thank you for saying that. I needed to hear it today.
I used to think being ‘stable’ meant never crying. Now I know it means crying-and still showing up.
You’re not alone.





christian Espinola
January 18, 2026 AT 06:42 AM
DBT? More like Dumb Behavior Training. They just teach you to breathe and hold ice cubes like a toddler having a tantrum. Real therapy digs into trauma, not gimmicks. And don’t get me started on the ‘homework’-like I don’t have enough to do already. This is just corporate wellness fluff repackaged as science.
Also, why is everyone acting like DBT is the only thing that works? I’ve seen people cured with EMDR, psychodynamic therapy, even just a good therapist who listens. But no, we gotta sell this 90s fad like it’s the Second Coming.
And don’t even mention the ‘phone coaching.’ That’s not therapy-that’s a crisis hotline with a fancy label. You’re paying $200/hour for someone to say ‘take a breath’? Come on.
Also, the stats? All from Linehan’s own studies. Where’s the independent replication? Where’s the control group that didn’t get the placebo of ‘skill worksheets’? I’ve seen too many people waste years on this.
It’s not that the skills are useless-it’s that they’re being sold as a cure-all when they’re just bandaids on a gunshot wound. And the tone of this post? Like it’s a religious text. Ugh.
Also, the ‘crisis plan’? I wrote mine on a napkin. It said ‘call mom.’ That’s it. And it worked better than all your TIPP charts combined.
Stop treating BPD like a DIY project. It’s not a spreadsheet you can optimize.
And who the hell wrote this? A DBT sales rep? Because I’m not buying.
Also, why are there no mentions of neurobiology? No mention of childhood attachment disruption as root cause? No, just ‘do this exercise.’ Pathetic.