
When you’re undergoing chemotherapy, every pill, supplement, or even grapefruit you eat could change how your treatment works. It’s not just about the cancer drug itself-it’s what else is in your body. A simple over-the-counter painkiller, a popular herbal supplement, or even your morning orange juice might interfere with your chemotherapy in ways you never expected. And the stakes? They’re life or death.
Why Chemotherapy Drug Interactions Are a Silent Threat
Cancer treatment is complex. Most patients don’t take just one drug. They’re on a mix of chemotherapy, pain meds, anti-nausea pills, blood thinners, antidepressants, and often a long list of supplements. The problem? These don’t always play nice together. In fact, over half of outpatient cancer patients experience at least one potential drug interaction, and one in three of those could lead to serious harm-like organ damage, treatment failure, or even death. A study of 278 cancer patients found that 40% had interactions that could affect how well their chemo worked. Another study showed that drug interactions may be responsible for up to 4% of deaths in hospitalized cancer patients. That’s not a small number. It’s not a rare accident. It’s a preventable risk that happens far too often. The real danger isn’t always obvious. You might feel fine. Your blood tests might look normal. But underneath, your body could be struggling. A drug might be making your chemotherapy too strong-or too weak. One moment you’re getting the full dose you need. The next, your body can’t process it right, and the cancer keeps growing.How These Interactions Actually Work
There are three main ways chemotherapy drugs interact with other substances: pharmacodynamic, pharmacokinetic, and pharmaceutical. Pharmacodynamic interactions happen when two drugs affect your body in similar or opposite ways. For example, if you’re taking cisplatin (a chemo drug) and another nephrotoxic medication, your kidneys can get hit twice as hard. The damage adds up. You might not notice until it’s too late. Pharmacokinetic interactions are more common-and more dangerous. These involve how your body absorbs, breaks down, or gets rid of drugs. Most of these happen through the liver’s cytochrome P450 enzyme system. Think of it like a busy highway. If two drugs try to use the same exit at the same time, they jam it up. One drug might get stuck, building up to toxic levels. Or it might not get processed at all, so it never works. Gemcitabine and cisplatin? They work well together because they target cancer cells in different ways. But if you take grapefruit juice with either of them? That’s a problem. Grapefruit contains chemicals that block the enzyme CYP3A4. That enzyme normally helps break down many chemo drugs. When it’s blocked, the drugs stay in your system longer than they should. Toxicity spikes. Side effects get worse. Then there’s the newer, less understood threat: immunological interactions. Immune checkpoint inhibitors like pembrolizumab or nivolumab are changing cancer treatment. But they don’t just target cancer-they turn your immune system loose. And when your immune system gets confused by other drugs, it can attack your liver, skin, or lungs. Cases of severe liver damage and life-threatening skin reactions have been linked to these drugs when taken with certain antibiotics, antifungals, or even common supplements.Oral Chemo Is Changing the Game
Ten years ago, most chemotherapy was given in the hospital through an IV. Now, about 25% of chemotherapy drugs in development are oral. That means more patients are taking chemo at home. More pills. More chances for mistakes. Oral chemo drugs like capecitabine, temozolomide, or ibrutinib are convenient-but they’re also more likely to interact with food, supplements, and other meds. Why? Because they’re absorbed through your gut. What you eat, when you eat it, and what else you take with it all matter. Take a patient on oral chemotherapy who starts taking turmeric for inflammation. Turmeric can interfere with liver enzymes. It might make the chemo less effective-or more toxic. The patient feels fine. No red flags. But weeks later, their cancer starts spreading. The chemo didn’t work because the supplement blocked it.The Supplement Trap
You’ve probably heard that supplements are “natural,” so they’re safe. That’s a myth. The VA Whole Health Library warns that supplements aren’t regulated like prescription drugs. They don’t have to prove safety or effectiveness before hitting store shelves. Labels can be wrong. Products can be contaminated. And many contain hidden ingredients that interact with chemo. Here are some common supplements that can be dangerous with chemotherapy:- Garlic, ginger, ginkgo biloba: Increase bleeding risk, especially if you’re on blood thinners like warfarin.
- St. John’s Wort: Speeds up liver metabolism, making many chemo drugs less effective.
- Green tea extract: Can interfere with bortezomib, a drug used for multiple myeloma.
- Bilberry, black cohosh, dong quai: May affect hormone-sensitive cancers like breast or prostate cancer.
- Fish oil, flaxseed, vitamin E: Can thin the blood and increase bruising or bleeding during treatment.
Age, Other Medications, and Your Body’s Changes
As you get older, your body changes. Your liver and kidneys don’t work as fast. Your body composition shifts. That means drugs stay in your system longer. And if you’re taking five or more medications-which is common for people over 65-you’re at much higher risk. A 2014 study of 244 cancer patients over 70 found that 75% had potential for serious drug interactions. That’s three out of four. And that was before the rise of immunotherapy and newer oral drugs. Antidepressants are another hidden risk. Tamoxifen, used for breast cancer, relies on a specific liver enzyme to become active. But many common antidepressants-like paroxetine and fluoxetine-block that enzyme. So the tamoxifen doesn’t work. And the cancer comes back. One in eight American women take antidepressants. One in eight get breast cancer. That’s a dangerous overlap.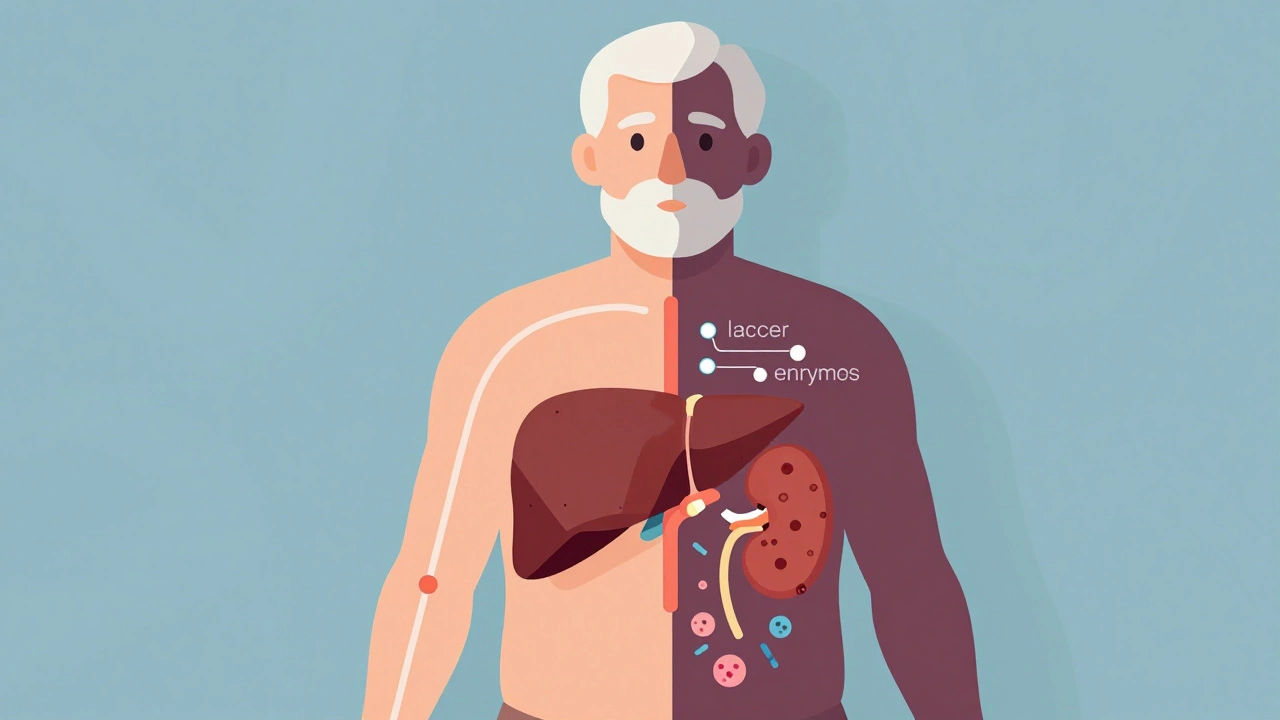
What You Can Do to Stay Safe
You don’t have to guess. You don’t have to risk it. Here’s what actually works:- Make a complete list. Write down every single thing you take: prescription drugs, over-the-counter meds, vitamins, herbs, teas, and even recreational substances. Include dosages and how often you take them.
- Share it with everyone. Give this list to your oncologist, pharmacist, and any other doctor you see. Don’t assume they know what you’re taking. They won’t ask unless you tell them.
- Ask about every new medication. Before you take anything new-even an OTC pain reliever like ibuprofen or acetaminophen-ask your pharmacist: “Is this safe with my chemo?”
- Stop supplements before surgery. If you’re having a procedure, stop all supplements at least 10 days before. Bleeding risks are real.
- Avoid grapefruit and Seville oranges. If you’re on chemo, skip them entirely. No exceptions.
- Use a pharmacist who specializes in cancer. Many hospitals have oncology pharmacists who track interactions daily. Ask if your clinic has one.
The Future: Personalized Safety
The good news? We’re getting better at this. Researchers are now using genetic testing to predict how you’ll process certain drugs. Some people have a version of the CYP2D6 gene that makes them slow metabolizers. For them, standard doses of tamoxifen or certain pain meds can be toxic. Testing for these variants is becoming more common. New software tools like Lexicomp and Micromedex now have oncology-specific interaction checkers. But they’re only as good as the data you feed them. If you forget to mention that you take turmeric daily, the system won’t warn you. And as immunotherapy becomes more common, we’re learning new rules. Some drugs that were once safe to combine with chemo are now dangerous with checkpoint inhibitors. We’re still figuring out which ones. That’s why ongoing communication with your care team is more important than ever.Final Word: Don’t Guess. Ask.
Chemotherapy is powerful. It saves lives. But it’s also fragile. One wrong pill, one extra supplement, one glass of grapefruit juice-and it can all fall apart. The system isn’t perfect. Doctors are busy. Pharmacists are stretched thin. But you’re the one who takes the pills. You’re the one who knows what’s in your body. Don’t be afraid to ask. Don’t assume something is safe just because it’s natural. Don’t wait until you feel sick to speak up. The safest way to fight cancer is to control every variable you can-including what you put in your mouth.Can I take ibuprofen while on chemotherapy?
It depends. Ibuprofen can increase bleeding risk, especially if you’re also on blood thinners or certain chemo drugs like cisplatin. It may also affect kidney function, which is already at risk with many chemotherapy agents. Always check with your oncology pharmacist before taking any NSAID, even over-the-counter ones.
Are herbal supplements safe during chemotherapy?
No, not without approval. Many herbal supplements interfere with how chemotherapy is processed by the liver or affect cancer cell responses. St. John’s Wort can make chemo less effective. Turmeric, garlic, and ginkgo can increase bleeding. Supplements aren’t regulated like drugs, so their contents can vary. Always tell your care team what you’re taking-even if you think it’s harmless.
Does grapefruit really affect chemotherapy?
Yes. Grapefruit and Seville oranges contain compounds that block the CYP3A4 enzyme, which is responsible for breaking down many chemotherapy drugs. This can cause drug levels to build up to toxic levels in your blood. Even one glass can have an effect that lasts for days. Avoid all grapefruit products while on chemo unless your oncologist says it’s safe.
Why do some cancer drugs stop working over time?
Cancer cells can develop resistance through several mechanisms: pumping drugs out of the cell, changing the drug’s target, or repairing DNA damage faster. Drug interactions can also play a role-if a supplement or other medication reduces the chemo’s effectiveness, the cancer may start growing again. That’s why tracking everything you take is critical.
What should I do if I accidentally take something that might interact with my chemo?
Call your oncology team right away. Don’t wait for symptoms. Even if you feel fine, the interaction might be happening inside your body. Your pharmacist can check if the interaction is major, minor, or unlikely to cause harm. They may adjust your dose, delay your next cycle, or monitor you more closely.
Staying safe during chemotherapy isn’t about being perfect. It’s about being informed. It’s about asking questions. It’s about not letting a simple mistake undo months of treatment. Your care team is there to help-but they need you to be honest, detailed, and proactive. Your life depends on it.
11 Comments
George Taylor
December 8, 2025 AT 23:36 PM
...I'm just saying... if you're going to die anyway, why bother with all these 'interactions'? You're already fighting cancer-why stress over grapefruit? Let the body do what it's gonna do. I mean, really... it's not like you're gonna live forever anyway. Just... chill.
ian septian
December 9, 2025 AT 18:13 PM
Write down everything. Give the list to your pharmacist. Ask before you take anything. That’s it. No magic. Just discipline.
Katherine Rodgers
December 11, 2025 AT 17:59 PM
ohhh so the 'natural' supplements that cost $40 a bottle are actually poison? shocker. next you'll tell me breathing oxygen can be dangerous if you're on chemo. wait-did someone already say that? oh right, the entire medical community. thanks for the hot take, doctor.
Lauren Dare
December 12, 2025 AT 04:47 AM
While the article correctly identifies pharmacokinetic interference via CYP3A4 inhibition, it fails to contextualize the clinical significance of these interactions. Many reported 'dangerous' interactions are based on in vitro data with supraphysiological concentrations. The real-world risk profile for most herbal supplements remains underpowered in prospective trials. Still, prudence dictates avoidance-especially in polypharmacy scenarios.
Darcie Streeter-Oxland
December 12, 2025 AT 19:00 PM
It is, indeed, a matter of considerable concern that patients are often left to self-regulate their intake of adjunctive substances without adequate professional oversight. The absence of mandatory reporting protocols for supplement use in oncology settings represents a systemic lacuna which, if unaddressed, may continue to result in preventable morbidity.
Sarah Gray
December 13, 2025 AT 07:46 AM
Anyone who takes 'natural' supplements while undergoing chemotherapy is either dangerously naive or actively self-sabotaging. You don’t get to play herbalist while your immune system is being nuked. If you’re going to risk your life, at least have the decency to be informed. Or better yet-don’t be that person.
Kathy Haverly
December 15, 2025 AT 06:58 AM
So what? You're telling me I can't have my green tea and my chemo? I'm already losing my hair, my appetite, and my dignity-now you want me to give up my matcha latte too? This is just medical gaslighting wrapped in a bullet list. I'll take my risk. And I'll die on my terms, not yours.
Suzanne Johnston
December 16, 2025 AT 01:37 AM
There’s a quiet tragedy here: we treat cancer like a war, but we treat the patient like a machine that can be calibrated with perfect inputs. What if the real problem isn’t grapefruit or turmeric-but a system that leaves people feeling so powerless they turn to anything that feels like control? Maybe the answer isn’t just more lists… but more compassion. And maybe, just maybe, we should stop scolding people for trying to survive with what little agency they have left.
Graham Abbas
December 16, 2025 AT 18:38 PM
I remember when my mom was on chemo… she swore by her ginger tea and turmeric paste. We didn’t tell the doctors. She was scared they’d say no. She lasted 18 months longer than they predicted. I don’t know if it was the supplements… or just her stubborn will to live. But I’ll never tell someone to stop hoping because of a drug interaction chart. Sometimes, the body knows more than the algorithm.
Haley P Law
December 18, 2025 AT 03:03 AM
OK but like… if I take a sip of grapefruit juice… am I gonna explode?? 😱 I’m just trying to enjoy my smoothie… this article gave me PTSD from my last chemo cycle… 🥲





Taya Rtichsheva
December 7, 2025 AT 15:46 PM
so i took turmeric for my knee and didn't tell my oncologist because i thought it was 'just a spice' now my chemo feels like it's working in slow motion and my bloodwork is weird af
oops