Most people don’t realize their kidneys are failing until it’s too late. That’s because chronic kidney disease (CKD) doesn’t scream for attention. No sharp pain. No fever. Just a quiet, slow decline - often unnoticed until the damage is severe. By the time symptoms like fatigue, swelling, or nausea show up, the kidneys may already be operating at 20% capacity. And here’s the hard truth: 90% of people with CKD don’t know they have it.
What Exactly Is Chronic Kidney Disease?
Chronic kidney disease isn’t a single illness. It’s a label for when your kidneys are damaged and can’t filter blood the way they should - and that damage lasts for at least three months. Your kidneys don’t just make urine. They balance your fluids, control blood pressure, produce red blood cell-stimulating hormones, and remove toxins. When they fail at these jobs, your whole body feels it. The standard way doctors measure kidney function is through something called eGFR - estimated glomerular filtration rate. It’s calculated from a simple blood test that checks creatinine levels. But eGFR alone doesn’t tell the whole story. That’s why doctors now combine it with another test: the albumin-to-creatinine ratio (ACR), which checks for protein leaking into your urine. Together, these two numbers create a full picture of your kidney health.The Six Stages of CKD: From Normal to Failure
The current system, updated by Kidney Disease: Improving Global Outcomes (KDIGO) in 2012, breaks CKD into five stages based on eGFR, plus three levels of albuminuria. It’s not just about how well your kidneys are working - it’s about how much damage is visible and how fast things are changing.- Stage G1 (eGFR ≥90): Your kidneys are filtering normally, but there’s proof of damage - like protein in your urine, structural issues seen on ultrasound, or scarring from a past infection. This stage isn’t about function. It’s about warning signs. Many people here have diabetes or high blood pressure and don’t realize their kidneys are already under stress.
- Stage G2 (eGFR 60-89): Kidney function is slightly reduced. Still, most people feel fine. This is where early detection matters most. If you have protein in your urine (ACR ≥30), you’re at higher risk of progression. A 2020 study found that people in G2 with high albuminuria were 3 times more likely to develop advanced CKD within five years.
- Stage G3a (eGFR 45-59): Mild to moderate loss. This is the turning point. Many doctors now recommend a nephrologist referral if you’re in G3a and have ACR >30. The SPRINT trial showed that starting an ACE inhibitor here can cut the chance of moving to Stage G4 by 37%.
- Stage G3b (eGFR 30-44): Moderate to severe decline. At this point, your risk of kidney failure jumps sharply. Patients in G3b are 2.6 times more likely to reach kidney failure within five years than those in G3a. Symptoms may start creeping in - swelling in ankles, trouble sleeping, or persistent itching.
- Stage G4 (eGFR 15-29): Severe loss. You’re now in the danger zone. Most people here are referred to a kidney specialist for dialysis or transplant planning. Your body is struggling to remove waste. Fluid builds up. Blood pressure gets harder to control. This is the last stage where you can still delay or avoid dialysis with aggressive care.
- Stage G5 (eGFR <15 or on dialysis): Kidney failure. At this point, your kidneys have lost nearly all function. Without dialysis or a transplant, toxins build up in your blood, and your body shuts down. Nearly 98% of people in G5 will eventually need one of these two life-saving treatments.
Albuminuria levels add another layer. A1 (normal) means less than 3 mg/mmol of protein in urine. A2 (3-30) is moderate. A3 (over 30) is severe. Someone with G3a and A3 albuminuria has a 5.4 times higher risk of dying early than someone with the same eGFR but normal urine protein.
Why Early Detection Makes All the Difference
The biggest problem with CKD? It’s silent. A 2022 survey by the National Kidney Foundation found that 78% of people diagnosed with Stage G2 or G3 had zero symptoms. They found out because their doctor ordered blood work for something else - a routine checkup, a knee surgery, or a diabetes screening. One patient, a nurse named Lisa from Ohio, found out she had Stage G3a after a routine urine test during a pre-op exam for knee replacement. She’d been blaming ankle swelling on standing all day. No one told her it could be her kidneys. “I thought I was healthy,” she said. “I ate well, walked every day. I didn’t even know kidneys could fail slowly like this.” When people are diagnosed early, they’re more likely to stick with treatment. A DaVita survey showed that patients diagnosed at Stage G3 or earlier had 32% better medication adherence and 41% more confidence managing their condition. They had time to learn, adjust, and prepare. Those diagnosed at G4 or later? They’re often scared, overwhelmed, and rushed into decisions. But here’s the flip side: some people panic when they get labeled with CKD at Stage G2. A UK study found that 22% of those patients felt anxious, even though their kidneys were still working well. That’s why doctors are now debating whether to call Stage G3a “CKD” at all - especially in older adults whose eGFR decline might just be aging, not disease.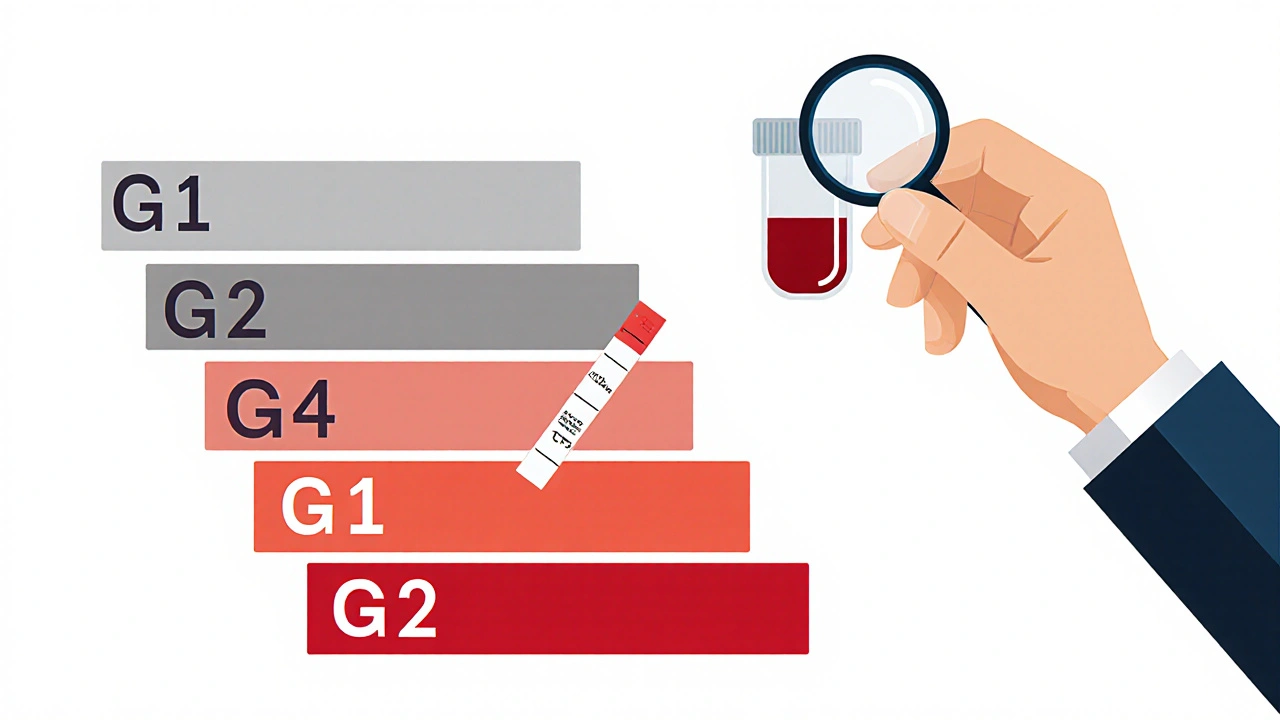
How Doctors Diagnose It - And Where They Miss It
The diagnosis isn’t complicated. Two things: a blood test for creatinine (to calculate eGFR) and a urine test for albumin (ACR). But here’s the catch: you need two abnormal results, at least 90 days apart. That’s to rule out temporary kidney stress - like dehydration, infection, or a bad reaction to medication. Many primary care doctors still miss CKD because they don’t check urine. Or they don’t know how to interpret the numbers. A Cleveland Clinic study found that when clinics added automated alerts in electronic records - flagging patients with eGFR under 60 and ACR over 30 - diagnosis rates jumped from 42% to 79% in just 18 months. But there are pitfalls. Sometimes, doctors mistake acute kidney injury (a sudden drop from illness or drugs) for chronic disease. That happens in 18% of cases, according to Mayo Clinic audits. Others overlook protein in the urine caused by conditions like multiple myeloma - a cancer that affects plasma cells. In 33% of early cases, this was missed because doctors only looked for albumin, not other proteins.Who’s at Risk - And Who Should Get Tested
Not everyone needs screening. But if you have any of these, get tested now:- Diabetes (37% of all CKD cases)
- High blood pressure (26% of cases)
- Heart disease
- Family history of kidney failure
- Being over 60
- Being African American, Native American, or Hispanic
African Americans are 3.5 times more likely to develop CKD than White Americans. Native Americans have the highest rates of diabetes-related kidney disease in the world - nearly half of those with diabetes will develop kidney damage.
Even if you don’t have risk factors, if you’re over 60, ask your doctor for a basic kidney check. eGFR naturally drops with age. But a sudden drop - more than 5 mL/min per year - is a red flag.
What You Can Do - Even If You’re Already in Stage G3
You can’t reverse kidney damage. But you can slow it down - sometimes dramatically.- Control blood pressure. Aim for under 130/80. ACE inhibitors or ARBs are often the first choice - they protect kidneys even if your blood pressure is normal.
- Manage blood sugar. If you have diabetes, keeping HbA1c under 7% cuts kidney damage risk by up to 30%.
- Stop smoking. Smoking narrows blood vessels in the kidneys. It’s one of the fastest ways to speed up decline.
- Avoid NSAIDs. Ibuprofen, naproxen, even high-dose aspirin can harm kidneys, especially if you’re already in G3 or higher.
- Watch your diet. Reduce salt. Limit processed foods. Don’t overdo protein unless your doctor says it’s okay.
- Get regular checkups. Every 6-12 months if you’re in G1-G3. Every 3 months if you’re in G4.
There’s no magic supplement. No herbal cure. The best thing you can do is follow the science - and stick with your treatment plan.
The Future: AI, Genes, and Better Screening
The field is changing fast. In 2023, the FDA approved the first AI tool - AION nephroTM - that predicts your kidney decline over the next two years with 88.7% accuracy. It looks at 27 factors: your age, blood pressure, lab values, even medications. Researchers are also testing genetic risk scores. A 2023 study in Nature Medicine found that 17 specific gene variants could predict who’s likely to progress quickly - with 92% accuracy. This could mean personalized screening: some people get tested every year, others every five. Community programs are also stepping up. The Baltimore Healthy Kidneys Initiative used mobile vans to test 5,832 people in high-risk neighborhoods. They found 1,247 previously undiagnosed cases - 43% of them in Stage G1 or G2. That’s thousands of people who got help before it was too late.What Happens If Nothing Changes?
Right now, Medicare spends $48 billion a year treating end-stage kidney disease. By 2030, that could hit $72 billion. Most of that cost comes from dialysis - which is expensive, exhausting, and life-altering. But if we catch CKD earlier and act, we can cut those costs. And more importantly, we can save lives. Every person diagnosed in Stage G2 or G3 has a chance to live years longer - with better quality - if they get the right care.You don’t need to wait for symptoms. You don’t need to be scared. You just need to know your numbers. Ask your doctor for an eGFR and ACR test. If you’re over 50, have diabetes, or high blood pressure - don’t wait. Your kidneys won’t warn you. But you can warn yourself.
Can chronic kidney disease be reversed?
No, kidney damage from chronic kidney disease can’t be reversed. But progression can often be slowed or stopped with proper treatment - especially if caught early. Controlling blood pressure, managing diabetes, avoiding harmful medications, and following a kidney-friendly diet can help preserve remaining function for years.
Do I need to see a kidney specialist if I’m in Stage G3?
Not always - but you should if your albuminuria is high (ACR >30), your eGFR is dropping quickly (more than 5 mL/min per year), or you have other complications like uncontrolled high blood pressure or anemia. Many primary care doctors manage Stage G3a well, but a nephrologist can help fine-tune treatment and plan for the future.
Is protein in urine always a sign of kidney disease?
Not always. Temporary protein in urine can happen after intense exercise, fever, or dehydration. But if it’s found twice, at least 90 days apart, it’s likely a sign of kidney damage. That’s why doctors require two abnormal tests before diagnosing CKD.
Can I still live a normal life with CKD?
Absolutely. Many people with Stage G1-G3 live full, active lives. The key is early detection and consistent management. Even those in Stage G4 can delay dialysis for years with good care. Focus on what you can control - diet, medications, blood pressure, and regular checkups.
Why is race no longer used in eGFR calculations?
Earlier eGFR formulas adjusted results for Black patients, assuming they had higher muscle mass. But this led to underdiagnosis in Black patients and delayed care. In 2021, the CKD-EPI equation was updated to remove race, making estimates more accurate and fair for everyone.
What’s the difference between eGFR and creatinine?
Creatinine is a waste product your muscles produce. Your kidneys filter it out. A blood test measures creatinine levels. eGFR is a number calculated from that creatinine level - along with your age, sex, and body size - to estimate how well your kidneys are filtering blood. eGFR tells you kidney function; creatinine is just one input.
Can I test for CKD at home?
There are home urine test strips that detect protein, but they’re not reliable enough for diagnosis. Blood tests for creatinine require a lab. The only way to get accurate eGFR and ACR results is through a doctor. Don’t rely on apps or over-the-counter kits - they can give false reassurance.
Does drinking more water help my kidneys?
For most people with CKD, drinking extra water doesn’t help kidney function. In fact, too much fluid can be dangerous if your kidneys can’t process it. Drink when you’re thirsty, but don’t force fluids unless your doctor says so. Balance matters more than volume.
14 Comments
Elizabeth Choi
November 28, 2025 AT 13:54 PM
90% don’t know they have it? That’s not a medical problem that’s a systemic failure of primary care.
Aishwarya Sivaraj
November 28, 2025 AT 21:33 PM
you know in india most people dont even get basic blood test unless they are really sick
and even then doctors check sugar blood pressure but rarely kidneys
my uncle had swelling in legs for 2 years they said its water retention from heat
turned out he was G4 and had no idea
we need awareness not just in usa but everywhere
and dont get me started on how expensive dialysis is here
Jebari Lewis
November 30, 2025 AT 03:05 AM
It is imperative to underscore the critical importance of the updated CKD-EPI equation that eliminates race-based adjustments in eGFR calculations. This represents a monumental advancement in equitable healthcare delivery. The prior methodology, which assumed higher muscle mass in Black patients, was not only scientifically unsound but also ethically indefensible. It resulted in delayed diagnoses, prolonged suffering, and increased mortality among marginalized populations. The correction of this systemic bias is not merely a statistical adjustment-it is a moral imperative. Furthermore, the integration of ACR with eGFR provides a more comprehensive diagnostic framework that enables early intervention. This paradigm shift in clinical practice must be aggressively promoted in all primary care settings. Delayed detection is not an accident-it is negligence.
Emma louise
December 1, 2025 AT 09:14 AM
Oh great another guilt trip for people who drink too much soda and eat fast food. So now my kidneys are my fault? What about the 200 pills they give you for blood pressure? Who’s really killing you here?
Alex Hess
December 3, 2025 AT 07:23 AM
This article is just a marketing pamphlet for nephrologists. Why are we even talking about eGFR? Just do a urine test and be done with it. All this jargon is just to make people feel like they need a specialist.
Lauren Zableckis
December 3, 2025 AT 09:54 AM
I think the most important takeaway is that CKD doesn’t have to be a death sentence. People can live well for years if they catch it early. It’s not about fear-it’s about awareness.
Asha Jijen
December 4, 2025 AT 14:13 PM
my cousin said he drinks 5 liters of water a day to flush his kidneys now he’s on dialysis
so much for internet wisdom
reshmi mahi
December 5, 2025 AT 11:08 AM
so if i drink lemon water every morning i can reverse G3a? 😏😂
laura lauraa
December 5, 2025 AT 16:12 PM
And yet… the system still fails. The system still ignores. The system still waits until the body screams before it listens. And when it does listen… it’s too late. Too late for the quiet ones. Too late for the ones who trusted the silence. Too late for the ones who didn’t know how to ask. And now… we’re all just waiting for the next one to disappear.
Gayle Jenkins
December 7, 2025 AT 09:25 AM
Stage G1 with protein in urine? That’s your wake-up call. Don’t wait. Don’t hope. Don’t think you’re fine. Start tracking your BP. Cut the salt. Get that ACR repeated. Talk to your doctor. You’re not broken-you’re being warned. And this is your chance to change the path.
Allison Turner
December 8, 2025 AT 21:13 PM
So if you’re Black, you used to get a pass on kidney disease? That’s just racism dressed up as science. And now they fixed it? Took long enough.
Darrel Smith
December 9, 2025 AT 01:34 AM
They took race out of the equation and now we’re all just numbers on a screen. What happened to the human touch? What happened to listening? Now it’s all labs and algorithms and no one even looks you in the eye anymore. This isn’t medicine. This is data collection.
Iives Perl
December 10, 2025 AT 15:38 PM
They’re hiding the truth. The real cause of CKD isn’t diabetes or high blood pressure. It’s the fluoride in the water. They don’t want you to know. Get your own test kit. Don’t trust the labs.






Kaleigh Scroger
November 27, 2025 AT 00:07 AM
Most people think if they feel fine their kidneys are fine but that’s the whole problem with CKD it creeps up like a shadow you don’t notice until it’s swallowing the sun
My mom was Stage G3b and didn’t know until she passed out from anemia they thought it was just aging turns out her creatinine had been creeping up for years
Doctors need to push eGFR and ACR together like they do with cholesterol not wait for symptoms
And yes protein in urine isn’t always kidney disease but if it’s there twice over 90 days you better get a nephrologist on speed dial
I’ve seen too many people get told to drink more water and come back in six months with G5 and no plan