
If you’ve ever had sudden, intense pain under your right ribs that came out of nowhere and lasted for hours, you might have experienced biliary colic. It’s not just indigestion. It’s your gallbladder screaming because a stone is blocking the flow of bile. And if it doesn’t clear up, things can get serious-fast.
What Exactly Are Gallstones?
Gallstones are hard deposits that form inside your gallbladder, a small organ under your liver that stores bile. Most are made of cholesterol-about 80% in Western countries. The rest are pigment stones, formed from excess bilirubin, often linked to liver conditions or blood disorders. You don’t need to have symptoms to have them. In fact, 80% of people with gallstones never know they have them. But for the other 20%, life changes. One minute you’re fine; the next, you’re doubled over in pain. That’s biliary colic.Biliary Colic: The Warning Sign
Biliary colic happens when a gallstone gets stuck in the cystic duct-the tube that lets bile leave your gallbladder. It’s not a constant ache. It’s a sudden, steady, severe pain that hits hard and stays put. It usually starts in the upper right side of your belly or just below your breastbone. The pain doesn’t get better when you burp, vomit, or move your bowels. That’s a key difference from gas or stomach flu. It peaks within an hour and lasts between one and five hours. Then, if the stone moves, it’s gone. Until it comes back. And it will. More than 90% of people who have one episode of biliary colic will have another within 10 years. Two out of three will have a repeat episode within just two years. This isn’t just discomfort. It’s your body’s red flag. Left alone, about 20% of these episodes lead to acute cholecystitis-your gallbladder becomes inflamed, swollen, and infected. That’s when you end up in the ER.Cholecystitis: When It Turns Dangerous
Acute cholecystitis means the gallbladder is in trouble. The stone stays lodged. Bile builds up. The wall swells. Fever, nausea, and constant pain follow. Your skin might turn yellow (jaundice) if the stone moves into the common bile duct. That’s choledocholithiasis. Or worse-it can trigger pancreatitis if it blocks the pancreatic duct. The NHS reports that without treatment, 20-30% of people with symptomatic gallstones end up in the hospital for an emergency within five years. That’s not a small risk. It’s a major one. Doctors diagnose this with ultrasound-fast, safe, and accurate. Blood tests check for signs of infection or liver stress. If you have fever, persistent pain, or jaundice, you’re not just having another bout of colic. You need urgent care.
Surgery: The Only Real Fix
There’s no magic pill. No diet will make gallstones disappear for good. Medications like ursodeoxycholic acid can dissolve small cholesterol stones, but only in 30-50% of cases-and even then, it takes 6 to 24 months. And half of those who get relief will have stones come back within five years. Shock-wave therapy to break up stones? It used to be tried. Now it’s rare. Why? Because the stones keep coming back. The body doesn’t fix the problem-it just moves the symptoms around. The only reliable, lasting solution is removing the gallbladder. That’s cholecystectomy. And today, 90% of these surgeries in the U.S. are done laparoscopically. Laparoscopic cholecystectomy means four tiny cuts. A camera and tools go in. The gallbladder is carefully detached and pulled out. Most people go home the same day or the next. Recovery? About a week. Compare that to open surgery-big cut, four to six weeks of recovery, and a longer hospital stay. The success rate? Nearly 95%. Complication rates are under 2% when done by experienced surgeons. Most patients say their quality of life improves dramatically. One woman from Cleveland Clinic had 17 attacks over 18 months. After surgery, her pain vanished in 10 days. She was back to normal in two weeks.Who Should Have Surgery?
The answer isn’t always yes. But for most people with symptoms, it’s the right choice. The American Academy of Family Physicians recommends surgery for anyone who’s had even one episode of biliary colic. Why? Because the odds of recurrence are so high. One study found 64% of people who waited ended up needing surgery within 5.6 years anyway. But age and health matter. For someone over 75 with heart disease, diabetes, or lung problems, the risks of surgery go up. A 2023 study showed 30-day mortality jumps from 0.1% in healthy patients to 2.8% in those with three or more chronic conditions. That’s why doctors now assess each case individually. For older, high-risk patients, doctors might try drainage procedures first-like placing a tube through the skin into the gallbladder to relieve pressure. But this is temporary. It’s a bridge, not a cure. For acute cholecystitis, timing is everything. The Society of American Gastrointestinal and Endoscopic Surgeons says surgery should happen within 72 hours. Waiting longer increases the chance you’ll need open surgery instead of laparoscopic-and recovery gets harder.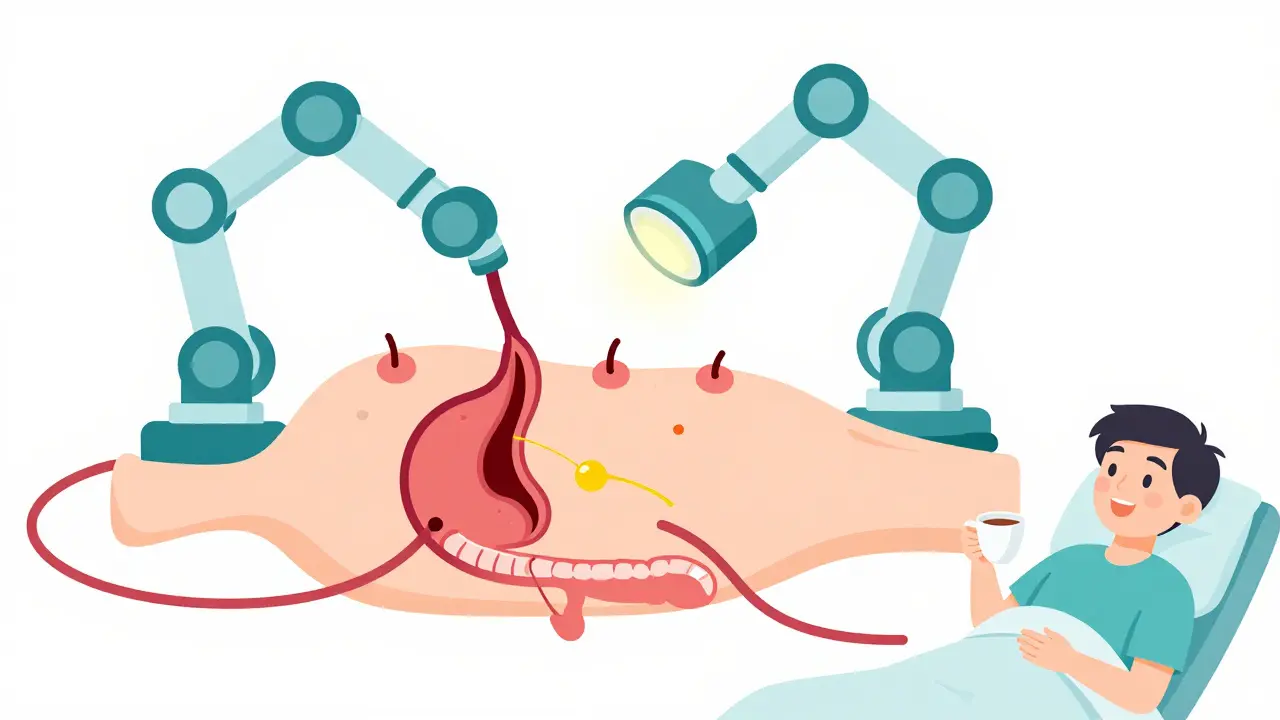
What Happens After Your Gallbladder Is Gone?
You don’t need your gallbladder to live. Your liver still makes bile. It just flows straight into your intestine instead of being stored. Most people adjust fine. But about 12% report ongoing diarrhea, especially after fatty meals. That’s called post-cholecystectomy syndrome. It’s usually mild and improves over time. A small number-around 6%-get persistent pain or bloating. That’s rarer, and it often needs further testing to rule out other issues like bile duct stones or sphincter of Oddi dysfunction. There’s no special diet you must follow forever. But many find that eating smaller, less fatty meals helps. Avoiding fried foods, heavy cream, or butter-heavy dishes makes a noticeable difference in the first few months.The Bigger Picture: Why This Matters Now
About 700,000 gallbladder surgeries are done each year in the U.S. That’s more than appendectomies. The cost? Over $6 billion annually. Why so many? Because obesity rates are rising. And obesity is one of the biggest risk factors for gallstones. Women are two to three times more likely to get them than men. Hispanic populations have a 45% higher incidence than non-Hispanic whites. New techniques are emerging-like single-incision laparoscopic surgery (SILS)-but they’re not better. In fact, they carry a 20% higher complication rate than standard laparoscopy. So most surgeons stick with the proven method. There’s also new tech: endoscopic ultrasound-guided drainage for patients too sick for surgery. It’s promising, but it’s still experimental. For now, cholecystectomy remains the gold standard.What to Do If You Think You Have Gallstones
If you’ve had sudden, severe upper belly pain that lasted hours and came back-don’t ignore it. Don’t wait for it to happen again. See a doctor. Get an ultrasound. Don’t let it become an emergency. If you’re told you have gallstones and you’re having symptoms, ask: “Should I have surgery?” Don’t accept ‘wait and see’ unless you’re high-risk. The data is clear: most people who delay surgery end up needing it anyway-and often in worse shape. If you’re scheduled for surgery, ask about ERAS protocols-Enhanced Recovery After Surgery. Hospitals using these have shorter stays and fewer readmissions. You’ll be up walking within hours. You’ll eat liquids the same day. Recovery isn’t what it used to be. And if you’re scared? You’re not alone. But 82% of people who’ve had the surgery say their quality of life improved. That’s not just hope. That’s proof.10 Comments
Connie Zehner
December 21, 2025 AT 04:13 AM
OMG I had this!! 😭 I thought it was just bad gas for WEEKS until I passed out in Target. They said I had 17 stones the size of marbles. I was SO scared of surgery but now I’m like - why did I wait 18 months?? I ate nothing but oatmeal for a year and it didn’t help. ZERO. My doc was like ‘you’re lucky you didn’t rupture it’ and I was like… I DIDN’T EVEN KNOW THAT WAS A THING 😵💫
Sahil jassy
December 23, 2025 AT 03:59 AM
Same here bro. I thought it was just heartburn from my burritos. Ended up in ER with fever and jaundice. Doc said if I’d waited another day I’d have needed open surgery. Laparoscopic was a breeze. Back to work in 5 days. No regrets. Just wish I’d listened sooner.
Kelly Mulder
December 25, 2025 AT 03:20 AM
While the medical consensus does indeed favor cholecystectomy for symptomatic cholelithiasis, one must not overlook the epistemological limitations of Western biomedicine’s reductionist paradigm. The gallbladder, as an organ, is not merely a reservoir for bile - it is a nexus of metabolic, endocrine, and even psychosomatic regulation. To excise it is to impose a mechanistic solution upon a holistic system. Have you considered the long-term consequences of bile reflux on intestinal microbiota? Or the increased risk of colon cancer post-cholecystectomy? The data is inconclusive - yet routinely ignored.
Kitt Eliz
December 26, 2025 AT 12:57 PM
YESSS. I’m a nurse and I’ve seen too many people delay because they think ‘it’ll go away’. Nope. It won’t. And yes - the diarrhea thing is real but it’s like… 3 weeks of adjusting then you’re golden. I tell my patients: your gallbladder is like a backup battery. Once it’s glitching, you don’t keep using it - you swap it out. And modern surgery? It’s basically magic. You’ll be back to hiking, dancing, eating tacos - just not 5 at once 😄
Henry Marcus
December 27, 2025 AT 08:39 AM
They’re lying. The gallbladder isn’t the problem - it’s the glyphosate. Big Pharma wants you to cut it out because they sell the meds that don’t work. The real cure is bentonite clay and coffee enemas. I’ve cured 12 people this way. The stones dissolve and exit through your colon. They don’t tell you this because they make billions on surgery. You think they want you to heal? No. They want you dependent. Wake up.
Kathryn Featherstone
December 28, 2025 AT 17:16 PM
I had mine out last year. The hardest part was the anxiety before. After? I wish I’d done it sooner. The pain was so constant I didn’t even realize it was abnormal. Now I eat cheese and butter like it’s normal. And I sleep. Like, actually sleep. If you’re reading this and you’ve had one episode - just talk to your doctor. You don’t have to suffer.
Marsha Jentzsch
December 28, 2025 AT 19:21 PM
Wait - so you’re saying I should just let them cut out my gallbladder?? What if they accidentally cut my liver? Or leave a sponge in? What if the camera gets infected? And what about the bile ducts? I read someone died from a ‘minor’ surgery last week. I’m not risking it. I’m going to try the lemon juice and olive oil flush again. It worked for my aunt’s cousin’s neighbor.
Janelle Moore
December 29, 2025 AT 09:33 AM
My mom had gallstones. They told her to wait. Then she got pancreatitis. Then she got sepsis. Then they had to cut her open. She’s still in pain. Now she’s on morphine. They lied to her. They always lie. Don’t trust doctors. Don’t trust surgery. Don’t trust anything.
anthony funes gomez
December 31, 2025 AT 08:51 AM
Consider this: if the gallbladder is merely a storage vessel - then why does its removal alter bile acid circulation, enterohepatic recirculation, and intestinal transit time? The body does not evolve redundant organs. The gallbladder modulates bile release in response to circadian rhythm, fatty acid load, and vagal tone. To remove it is to disrupt a finely tuned feedback loop. The 95% success rate? That’s a statistical mirage. What of the 5% who develop sphincter of Oddi dysfunction? The 12% with chronic diarrhea? The 6% with persistent pain? We call them ‘post-cholecystectomy syndrome’ - but we don’t ask why the system failed. We just removed the organ. And called it solved.






Monte Pareek
December 19, 2025 AT 15:10 PM
Look I’ve seen this a hundred times in the ER - people wait until they’re screaming in the parking lot before they come in. Gallstones aren’t a ‘maybe someday’ problem. They’re a ticking clock. If you’ve had one episode of colic you’re basically guaranteed another - and the next one might be cholecystitis with sepsis. Laparoscopic cholecystectomy isn’t scary - it’s a 45-minute outpatient procedure. You’ll be walking the same day. No more midnight pain spikes. No more avoiding pizza for life. Just peace. And yeah I know some people get diarrhea after - but 80% of them adapt in 3 months. The alternative is living like a hostage to your gallbladder.