
Diabetic neuropathy isn’t just numbness or tingling-it’s burning, stabbing, or electric shock-like pain that can make walking, sleeping, or even wearing socks unbearable. For millions with type 1 or type 2 diabetes, this nerve damage doesn’t go away with better blood sugar control alone. That’s where amitriptyline comes in-not as a cure, but as one of the most studied and effective tools to quiet the noise in damaged nerves.
What Is Amitriptyline, Really?
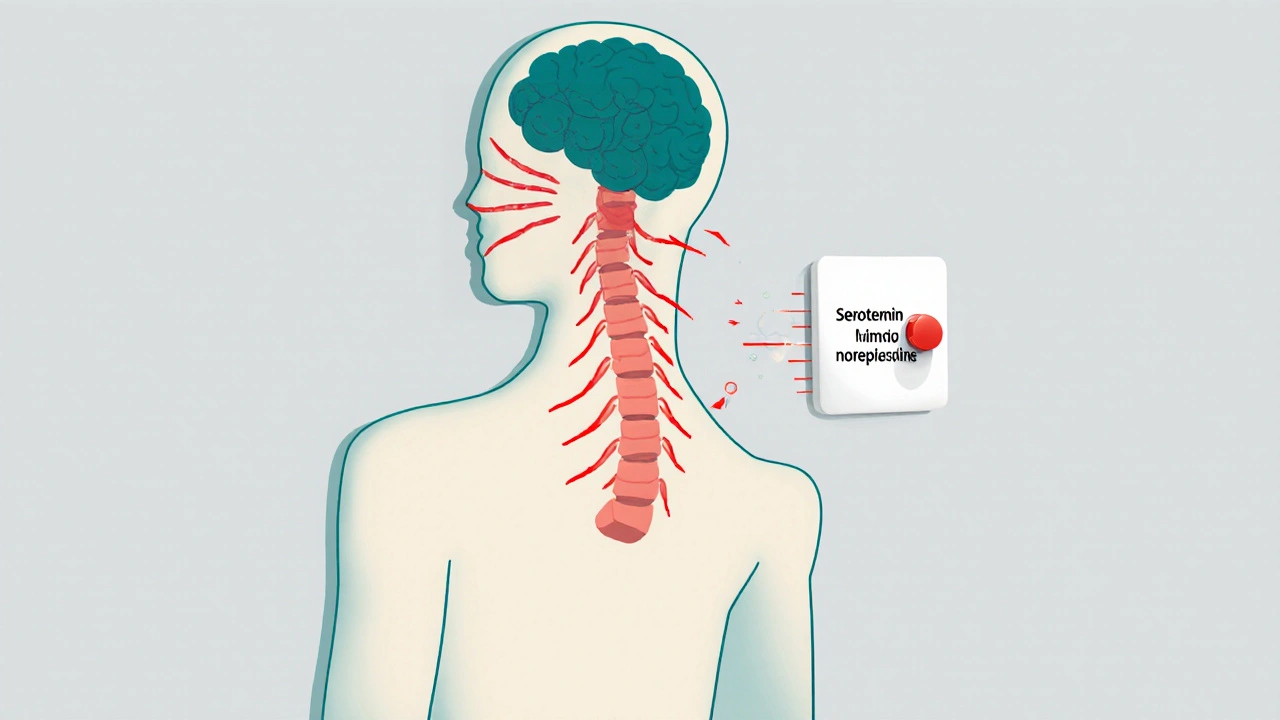
Amitriptyline is an older tricyclic antidepressant, first approved in the 1960s. But for diabetic neuropathy, it’s rarely used because someone is depressed. It’s used because it changes how the brain and spinal cord process pain signals. At low doses-often just 10 to 50 mg a night-it blocks the reuptake of serotonin and norepinephrine, two chemicals that help dampen pain messages before they reach your conscious mind.
Unlike painkillers like ibuprofen or even opioids, amitriptyline doesn’t target inflammation or block pain receptors directly. Instead, it rewires the way your nervous system interprets signals from damaged nerves. Think of it like turning down the volume on a broken speaker that’s screeching nonstop.
Why Amitriptyline Works for Nerve Pain
Studies show that amitriptyline reduces diabetic neuropathy pain by about 30 to 50% in people who respond to it. A 2023 meta-analysis of 12 randomized trials found that patients taking amitriptyline were twice as likely to report at least a 50% reduction in pain compared to those on placebo. These results aren’t just statistical-they’re lived. People describe it as the difference between constant fire and a manageable warmth.
It works best for burning, shooting, or tingling pain, which are classic signs of small fiber neuropathy. If your pain feels more like muscle cramps or joint stiffness, amitriptyline might not be the right fit. That’s why doctors don’t hand it out like candy-they look for the right pain pattern first.
How It’s Actually Taken
You won’t start at 150 mg. That’s the old antidepressant dose. For nerve pain, doctors begin with 10 mg at bedtime. Why bedtime? Because amitriptyline makes most people drowsy. That side effect becomes a benefit here-you’re treating pain and helping sleep at the same time.
It takes time. Most people don’t feel relief until after 2 to 4 weeks. Some need up to 8 weeks. If there’s no improvement by then, your doctor will likely stop it. If it works, you’ll stay on the lowest effective dose, often for months or even years. You don’t suddenly stop it either. Tapering down slowly over weeks prevents withdrawal symptoms like nausea, headaches, or rebound pain.
Side Effects You Need to Know
Not everyone tolerates amitriptyline. The most common side effects are dry mouth, constipation, blurred vision, dizziness, and weight gain. These aren’t rare-they happen in up to 40% of users. But many learn to live with them. Sipping water, chewing sugar-free gum, and increasing fiber can help.
More serious risks include heart rhythm changes, especially in people over 60 or those with existing heart conditions. That’s why doctors often check an ECG before starting, especially if you’re older or have a history of heart issues. It’s also not safe with certain medications like MAO inhibitors or some antiarrhythmics.
People with glaucoma, enlarged prostate, or severe liver disease are usually advised against it. If you’re pregnant or breastfeeding, talk to your doctor-there’s limited data, and risks aren’t fully understood.
How It Compares to Other Options
Amitriptyline isn’t the only game in town. Here’s how it stacks up against other common treatments:
| Treatment | Typical Dose | Time to Effect | Common Side Effects | Effectiveness for Nerve Pain |
|---|---|---|---|---|
| Amitriptyline | 10-75 mg nightly | 2-8 weeks | Drowsiness, dry mouth, weight gain | High (30-50% pain reduction) |
| Gabapentin | 300-1,800 mg daily | 1-4 weeks | Dizziness, swelling, fatigue | High (30-40% reduction) |
| Pregabalin | 75-300 mg daily | 1-2 weeks | Dizziness, weight gain, blurred vision | High (40-50% reduction) |
| Duloxetine | 60 mg daily | 2-4 weeks | Nausea, fatigue, dry mouth | High (30-45% reduction) |
| Topical capsaicin | 0.075% cream, 3-4x/day | 2-6 weeks | Burning sensation (temporary) | Moderate (20-30% reduction) |
Amitriptyline is often cheaper than gabapentin or pregabalin, especially in generic form. But duloxetine, an SNRI like amitriptyline, has fewer anticholinergic side effects and is FDA-approved specifically for diabetic neuropathy. Still, many patients respond better to amitriptyline-even when other drugs fail.
Who Should Avoid It
Not everyone is a candidate. If you’ve had a heart attack in the past year, have uncontrolled glaucoma, or take certain antidepressants like selegiline, amitriptyline is off-limits. People with a history of seizures should use it cautiously. Older adults are more sensitive to its effects on balance and memory, so doctors start even lower-sometimes 5 mg-and move slowly.
If you’ve tried other treatments and still have pain, amitriptyline might be worth discussing. But if you’re already on multiple medications, your pharmacist should check for interactions. It can boost the effects of alcohol, benzodiazepines, and some blood pressure drugs.
Real-Life Success Stories
One 62-year-old man from Auckland, diagnosed with type 2 diabetes for 18 years, couldn’t sleep because his feet felt like they were on fire. He’d tried gabapentin, but the dizziness made him fall. His doctor switched him to 25 mg of amitriptyline at night. Within three weeks, his pain dropped from an 8/10 to a 3/10. He started walking again. He still takes it, five years later.
A woman in Christchurch, 54, with diabetic neuropathy in her hands, couldn’t button her shirts or hold a coffee cup. After six weeks on 10 mg of amitriptyline, she regained enough sensation to type again. She says it didn’t erase the pain-but it made it bearable.
These aren’t outliers. They’re common outcomes when the drug is used correctly: low dose, slow start, patience, and monitoring.

What Happens If It Doesn’t Work?
About 30% of people don’t respond to amitriptyline. That doesn’t mean you’re out of options. You might try duloxetine, pregabalin, or topical lidocaine patches. Some combine treatments-like low-dose amitriptyline with capsaicin cream. Others turn to non-drug options: physical therapy, acupuncture, or even transcutaneous electrical nerve stimulation (TENS).
It’s also worth checking if your blood sugar is truly under control. Sometimes, pain improves just by getting HbA1c below 7%. But even then, nerve damage can linger. That’s why treatment is often layered-not one drug, but a plan.
Long-Term Use and Safety
Many people take amitriptyline for years without issues. But long-term use can lead to tolerance-meaning you might need a small dose increase over time. Weight gain is the most common concern, and it can worsen insulin resistance. That’s why diet and movement are still part of the plan.
Regular check-ins with your doctor are key. Blood tests for liver function, heart rhythm checks, and weight monitoring should happen every 6 to 12 months. You’re not just managing pain-you’re protecting your whole health.
Final Thoughts
Amitriptyline isn’t flashy. It’s not new. But for diabetic neuropathy, it’s one of the most reliable tools we have. It doesn’t fix the nerve damage. But it can give you back your nights, your steps, your ability to live without constant discomfort.
If you’re struggling with nerve pain and haven’t tried it, talk to your doctor. Ask about starting low, going slow, and what to expect. Don’t give up if it takes weeks. And don’t quit because of side effects-you can often manage them.
This isn’t about taking a pill to feel normal. It’s about taking a small step toward feeling like yourself again.
Can amitriptyline cure diabetic neuropathy?
No, amitriptyline doesn’t cure diabetic neuropathy. It doesn’t repair damaged nerves. What it does is reduce the pain signals those damaged nerves send to your brain. It helps you manage symptoms, not reverse the condition. Controlling blood sugar remains the only way to slow or stop nerve damage from getting worse.
How long does it take for amitriptyline to work for nerve pain?
Most people start noticing less pain after 2 to 4 weeks, but it can take up to 8 weeks to feel the full effect. This is slower than painkillers like ibuprofen, but the relief lasts longer and targets the root of nerve pain, not just surface inflammation. Patience is key.
Is amitriptyline addictive?
Amitriptyline is not addictive in the way opioids or benzodiazepines are. You won’t crave it or get high from it. But if you stop suddenly, you can get withdrawal symptoms like nausea, headaches, or increased pain. That’s why you must taper off slowly under medical supervision.
Can I drink alcohol while taking amitriptyline?
It’s not recommended. Alcohol makes the drowsiness and dizziness from amitriptyline much worse. It also increases the risk of falls, especially in older adults. Even one drink can throw off your balance. If you choose to drink, do so very rarely and in tiny amounts-and always talk to your doctor first.
Are there natural alternatives to amitriptyline for neuropathy?
Some people find relief with alpha-lipoic acid, acetyl-L-carnitine, or capsaicin cream. Physical therapy and TENS units can also help. But none have as much strong evidence as amitriptyline. Natural doesn’t always mean better. Always check with your doctor before trying supplements-they can interact with other meds.
Will I need to take amitriptyline forever?
Not necessarily. Some people stay on it long-term because their pain returns if they stop. Others reduce the dose after months or years and manage well. It depends on how severe your nerve damage is and whether your blood sugar control has improved. Your doctor will help you decide when, or if, to stop.
Next Steps
If you’re considering amitriptyline, start by asking your doctor these questions: Has my pain pattern been assessed? Have my heart and liver been checked? What’s the lowest dose I can start with? What side effects should I watch for? How will we know if it’s working?
Keep a pain journal. Note your pain level each day, your sleep quality, and any side effects. That data helps your doctor adjust your dose faster and smarter.
And don’t forget the basics: check your feet daily, wear proper shoes, control your blood sugar, and move every day. Amitriptyline helps you live better-but it doesn’t replace the foundation of diabetes care.
11 Comments
Nick Zararis
October 31, 2025 AT 03:04 AM
Start low. Go slow. Monitor. Document. Adjust. Don't quit too soon. Don't rush the taper. Talk to your pharmacist. Check your ECG. Track your HbA1c. Sleep hygiene matters. Hydration helps with dry mouth. Fiber combats constipation. Avoid alcohol. Avoid grapefruit. Avoid sudden changes. Be patient. It takes time. It's not magic. But it works-for a lot of people.
And if it doesn't? Then try the next thing. But don't dismiss the tool just because it's old.
Sara Mörtsell
November 1, 2025 AT 23:26 PM
Everyone acts like amitriptyline is this miracle drug but let's be real-it's a chemical sedative with side effects that make you feel like a zombie who forgot how to blink. I've seen people gain weight, forget their grandkids' names, and fall down stairs because they were too drowsy to walk straight. Why are we glorifying this? We're just trading one kind of suffering for another.
And don't even get me started on 'it's not addictive'-you think withdrawal isn't real? You think your nerves don't scream when you stop? It's just a different kind of addiction-pharmaceutical Stockholm syndrome.
Rhonda Gentz
November 3, 2025 AT 18:44 PM
There's something deeply human about how we treat pain. We want a cure, a reset button, a fix. But nerve damage doesn't care about our desire for closure. Amitriptyline doesn't heal-it softens. It doesn't erase the fire, it teaches you how to sit beside it without being consumed.
I think that's why it works for so many. Not because it's powerful, but because it's gentle. It doesn't promise salvation. It just says: 'You don't have to be destroyed by this anymore.'
That's enough.
Alexa Ara
November 3, 2025 AT 19:43 PM
For anyone considering this-don't panic about side effects. Start at 10mg. Take it at night. Drink water. Chew gum. Walk around the house before bed. You'll be fine. I was scared too. Now I'm five years in, sleeping through the night, and actually able to hug my kids without wincing.
You're not weak for needing this. You're brave for trying it.
❤️
Olan Kinsella
November 4, 2025 AT 22:26 PM
Let me tell you about my cousin in Lagos-he took amitriptyline for three months, stopped because he thought it was 'making him weak,' then his feet caught fire again. He went to a herbalist who gave him 'diabetic root tea' and a chicken sacrifice. He died last year. His family blamed the drug. I blame ignorance.
People think traditional medicine is pure. But when you're in pain, you'll swallow anything. This isn't about culture. It's about science. And science says: amitriptyline saves lives. Not always perfectly. But often enough to matter.
Chris Dockter
November 6, 2025 AT 19:27 PM
Wow another article fawning over a 60-year-old tricyclic antidepressant like it's the holy grail. Gabapentin's cheaper, pregabalin's faster, duloxetine's FDA-approved, and capsaicin's topical. Why are we still pushing this dinosaur? It's like recommending a flip phone because it 'never crashes.'
Also-'low dose'? That's what they say when they don't want to admit they're just dosing people into oblivion so they stop complaining. Wake up. This isn't medicine. It's chemical suppression.
Gordon Oluoch
November 8, 2025 AT 14:04 PM
Let's not pretend this is a benign treatment. Amitriptyline has a black box warning for suicidal ideation in young adults. It prolongs QT intervals. It interacts with 87% of common cardiac meds. And yet doctors prescribe it like it's aspirin. Where's the accountability? Where's the informed consent? People are being medicated into silence because the system doesn't have time to explore alternatives.
This isn't care. It's convenience wrapped in a placebo narrative about 'quieting the noise.'
And don't even get me started on the 'real-life success stories.' They're cherry-picked. The ones who died from arrhythmias? They're not in the article. The ones who quit because they couldn't lift their arms? Also not mentioned.
This is pharmaceutical propaganda disguised as patient advocacy.
April Liu
November 9, 2025 AT 21:28 PM
I've been on this for 3 years. Dry mouth? Yeah. Weight gain? A little. But I can wear socks again. I can hug my granddaughter without crying. I didn't know pain could be this quiet until it was.
And honestly? I'm not ashamed to say this pill gave me back my life. If you're scared-start low. Talk to your doctor. Keep a journal. You got this.
💛
Emily Gibson
November 10, 2025 AT 02:04 AM
For those of you scared to start this-remember: you're not broken. You're not weak. You're just a person with damaged nerves trying to live in a world that doesn't understand invisible pain.
Amitriptyline isn't about being fixed. It's about being held. And sometimes, that's enough.
You're not alone.
Mirian Ramirez
November 10, 2025 AT 11:29 AM
i started on 10mg and thought i was gonna die from the drowsiness but after two weeks i was sleeping like a baby and my feet stopped feeling like they were dipped in hot oil. i still get dry mouth but i carry a water bottle everywhere and chew gum like its my job. my doc said i might be on it forever but honestly? i dont care. i can walk to the mailbox again. i can hold my coffee without dropping it. i dont need a miracle. i just needed to not be in constant pain.
also i typoed half this comment because i was typing with one hand while holding my cat who is now asleep on my lap. life is good.




Herbert Lui
October 29, 2025 AT 08:55 AM
amitriptyline is one of those old-school drugs that somehow still works better than half the new stuff. i remember my uncle on it for 12 years-dry mouth, weighed 30 lbs more, but he could finally sleep without screaming. sometimes medicine isn't about flashy breakthroughs-it's about quiet, stubborn relief.
and yeah, it's not a cure. but for people who've lost their nights to burning feet? it's a lifeline wrapped in a pill.