
Chronic Diarrhea and Intimacy Impact Calculator
Your Impact Assessment
Living with chronic diarrhea is more than just an inconvenient bathroom schedule. It can sneak into the bedroom, the dinner table, and the bedtime conversation, leaving both partners feeling frustrated, embarrassed, or withdrawn. This article breaks down why the condition reaches into your personal life, what you can do together to keep the spark alive, and when professional help is the best move.
Key Takeaways
- Frequent bathroom trips can trigger stress, lower self‑esteem, and disrupt intimacy.
- Open communication and practical planning are the most effective fixes.
- Diet tweaks, medication, and probiotics can reduce symptoms for many people.
- Therapy or medical consultation is essential if symptoms or emotional strain persist.
What Is Chronic Diarrhea?
Chronic diarrhea is defined as loose, watery stools that occur three or more times a day for at least four weeks. It can stem from infections, inflammatory bowel disease, irritable bowel syndrome, medication side‑effects, or food intolerances. The daily uncertainty-wondering when the next urgent trip will be-creates a hidden emotional load that spills over into every relationship arena.
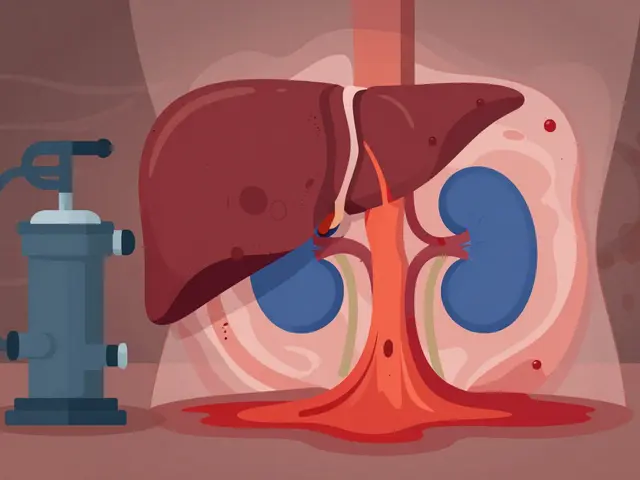
How the Gut Talks to Your Heart (and Bedroom)
Gut health isn’t just about digestion; it’s a major player in mood regulation. Gut health influences the production of serotonin, the ‘feel‑good’ neurotransmitter, by up to 90% of the body’s total. When chronic diarrhea disrupts that balance, you can feel more anxious, irritable, or fatigued-states that make closeness feel like a chore.
Intimacy, in turn, thrives on confidence and physical comfort. Intimacy is the blend of emotional closeness, sexual connection, and physical touch that partners share. Persistent digestive symptoms can lower self‑esteem, cause fear of odor or accidents, and lead partners to avoid cuddling or sex altogether.
At the relationship level, the pattern often looks like this: frequent trips → heightened stress → reduced desire → emotional distance → more stress. Breaking the cycle requires deliberate action on both sides.
Talking About It Without Blushing
Many couples avoid the topic because it feels “gross” or “embarrassing.” Yet the hidden conversation does more damage. Here’s a simple script to start the dialogue:
- Pick a calm moment-not right after a bathroom run.
- Use “I” statements: “I feel anxious when I’m not sure I’ll make it to the bathroom in time.”
- Invite your partner’s perspective: “How does this affect you?”
- Agree on one small adjustment to try this week.
Practice makes perfect. The more you talk, the less the subject feels like a secret.

Practical Strategies to Keep Things Flowing
Below is a quick‑reference table that matches common coping tactics with their typical impact on intimacy.
| Strategy | How It Helps Symptoms | Effect on Intimacy |
|---|---|---|
| Low‑FODMAP diet | Reduces gas and loose stools for many IBS patients | Fewer urgent trips → more confidence during sex |
| Prescription anti‑diarrheal meds (e.g., loperamide) | Slows bowel movement frequency | Allows longer uninterrupted moments |
| Probiotic supplement | Balances gut microbiome, may lower frequency | Improves overall mood, boosting closeness |
| Scheduled “safe” times for intimacy | None directly | Reduces anxiety about sudden episodes |
| Use of waterproof sheets & quick‑wipe wipes | None directly | Minimises stress over accidental leaks |
Pick one or two that feel doable and try them for a week. Small wins add up fast.
When Diet and Meds Aren’t Enough
If symptoms linger despite lifestyle changes, it’s time to bring in professionals. Medication such as prescription antispasmodics, bile acid binders, or even biologics can target underlying inflammation. A gastroenterologist can run tests to rule out infections, celiac disease, or ulcerative colitis.
Equally important is mental health support. Stress amplifies gut motility, creating a feedback loop where anxiety worsens diarrhea, and diarrhea fuels anxiety. A therapist versed in chronic illness coping can teach relaxation techniques, cognitive reframing, and couples counseling.
Checklist for Couples Dealing with Chronic Diarrhea
- Schedule a weekly check‑in to discuss symptoms and feelings.
- Identify dietary triggers together (keep a simple food‑symptom log).
- Keep bathroom essentials (soft toilet paper, wipes) handy in the bedroom.
- Invest in breathable, easy‑to‑wash bedding.
- Set a ‘no‑phone’ moment before intimacy to focus on connection, not symptoms.
- Plan a “backup” activity if a sudden episode occurs (e.g., a short walk, a funny video).
- Visit a healthcare provider if stools are watery for >4 weeks, contain blood, or cause weight loss.
Bottom Line
The physical toll of chronic diarrhea is real, but the emotional fallout doesn’t have to dictate the future of your relationship. By talking openly, tweaking diet and medication, and using practical tools to protect intimacy, couples can stay close even when the bathroom seems to have a front‑row seat.
Frequently Asked Questions
Can chronic diarrhea affect my libido?
Yes. The constant discomfort, fatigue, and worry about accidents can lower sexual desire. Addressing symptoms and communicating needs often restores libido.
Is it safe to use over‑the‑counter antidiarrheal pills?
For short‑term relief they’re usually fine, but they don’t treat underlying causes. If you need them daily, see a doctor to avoid masking a serious condition.
Do probiotics really help?
Evidence shows certain strains (like Bifidobacterium infantis) can reduce IBS‑related diarrhea in about 30‑40% of users. It’s worth trying a reputable brand for at least a month.
How can I make intimacy more comfortable on a bad day?
Focus on non‑penetrative affection: cuddling, massage, or whispering. Use waterproof bedding and keep wipes nearby. Small gestures keep the connection alive without pressure.
When should I see a gastroenterologist?
If loose stools last more than four weeks, cause weight loss, blood, or severe pain, schedule an appointment. Early diagnosis can prevent complications and improve quality of life.
20 Comments
lee charlie
October 4, 2025 AT 00:20 AM
I hear you, and it’s true that being open can actually bring you closer. When you share the practical side, like when the “worst” times are, it removes the mystery and lets you both plan. It also shows trust, which is a huge intimacy booster.
Joy Luca
October 4, 2025 AT 19:46 PM
Exactly-transparency builds a shared roadmap. In clinical terms, this is called “symptom‑trigger mapping,” and it gives both partners data to work with. Over time, the brain learns to associate intimacy with safety rather than anxiety.
Jessica Martins
October 5, 2025 AT 15:13 PM
Thanks for laying out these strategies so clearly. It’s helpful to see both the emotional and logistical sides covered.
Greg DiMedio
October 6, 2025 AT 10:40 AM
Oh great, another “let’s talk about poo” moment.
Jarod Wooden
October 7, 2025 AT 06:06 AM
From a psychosomatic perspective, chronic diarrheal episodes can be conceptualized as a dysregulated neurogastroenteric axis, wherein stress hormones perpetuate epithelial permeability. This bi‑directional feedback loop not only compromises physical comfort but also recalibrates affective attunement between dyadic partners. The resultant cognitive load may manifest as perceived relational distance, a phenomenon well documented in the psychoneuroimmunology literature.
Brenda Hampton
October 8, 2025 AT 01:33 AM
I’m curious about how often couples actually sit down and schedule “intimacy windows” around health issues. Does that feel like a compromise or a partnership win?
Scott Davis
October 8, 2025 AT 21:00 PM
It’s a trade‑off, but teamwork beats silence.
Doug Farley
October 9, 2025 AT 16:26 PM
Yeah, because nothing says romance like a bathroom sprint.
Marcella Kennedy
October 10, 2025 AT 11:53 AM
Living with chronic diarrhea can be a relentless undercurrent that seeps into every facet of a relationship, and the first step is acknowledging its pervasive impact without shame. When you admit that the condition shapes your daily routine, you give your partner permission to step into the reality of your life, which is far more intimate than any bedroom encounter. Practical measures-like having a “symptom kit” ready with wipes, spare underwear, and discreet medication-can alleviate the logistical anxiety that often hangs over spontaneous moments. Moreover, discussing the timing of intimacy when you anticipate lower symptom frequency can turn what feels like a gamble into a planned, enjoyable experience. Emotional support is just as crucial; a partner who listens without judgment creates a safe harbor that can reduce the stress‑induced flare‑ups that exacerbate the condition. It’s also important to cultivate non‑physical forms of closeness, such as shared hobbies, deep conversations, or even simple gestures like holding hands, which reinforce the bond when physical intimacy is temporarily limited. Over time, these strategies help rewire the brain’s association of intimacy from fear of embarrassment to a feeling of security. Couples therapy can offer a neutral space to explore these dynamics, and many therapists specialize in chronic illness coping mechanisms. Nutrition and lifestyle tweaks-like low‑FODMAP diets or stress‑reduction techniques-can further diminish symptom severity, giving you more wiggle room for closeness. Remember that intimacy is a spectrum; the goal isn’t to maintain a constant high‑frequency physical schedule but to nurture a resilient connection that can weather health storms. When both partners view the condition as a shared challenge rather than a personal flaw, the relationship often emerges stronger. Celebrate small victories, such as a symptom‑free evening, and let those moments reinforce your collective resilience. Keep communication lines open, using “I” statements to express how you feel without placing blame. In doing so, you model vulnerability, which is the true catalyst for deep intimacy. Finally, be patient with yourselves; healing, adjustment, and acceptance are processes that evolve over weeks and months, not days.
Pam Mickelson
October 11, 2025 AT 07:20 AM
Great points! Adding humor to the mix can also lighten the mood and remind both of you that you’re in this together.
Calvin Smith
October 12, 2025 AT 02:46 AM
Honestly, turning a bathroom marathon into a lyrical duet might just be the next big thing in relationship hacks-who’s with me?
Donnella Creppel
October 12, 2025 AT 22:13 PM
Wow, this is sooo typical!! Everyone acts like chronic diarrhea is the end‑of‑the‑world crisis we all need to panic over… Really? Can we just move on??!!!
Jeremy Olson
October 13, 2025 AT 17:40 PM
In my experience, maintaining a formal tone when discussing health concerns can help keep the conversation objective and reduce emotional escalation.
Ada Lusardi
October 14, 2025 AT 13:06 PM
Sending you lots of love and good vibes 💙✨ Stay strong!
Joe V
October 15, 2025 AT 08:33 AM
Sure, let’s all act like this is just a minor inconvenience, while ignoring the real strain it puts on daily life. Classic.
Matt Stone
October 16, 2025 AT 04:00 AM
Deal with it or quit whining.
Lara A.
October 16, 2025 AT 23:26 PM
Honestly, the government’s agenda on “gut health” is a cover‑up for mass surveillance of bowel movements-don’t believe the mainstream narrative!
Ashishkumar Jain
October 17, 2025 AT 18:53 PM
Yo, i think we can hack this situation by syncin our schedules and keepin it lowkey. It’s all bout dat trust, man.
Gayatri Potdar
October 18, 2025 AT 14:20 PM
They’re hiding the truth about how “probiotic” scams are actually mind‑control tools. Wake up, people!




christian quituisaca
October 3, 2025 AT 04:54 AM
First off, dealing with chronic diarrhea can feel like walking on a minefield when intimacy comes up. It’s completely normal to feel self‑conscious, but communication with your partner is the cornerstone of navigating this challenge. Try framing the conversation around your needs and boundaries, rather than the embarrassment. When you articulate how symptoms affect you, your partner can become an ally rather than an obstacle. Small adjustments-like timing intimacy after a low‑symptom window or keeping a spare set of supplies nearby-can preserve the emotional connection. Remember, intimacy isn’t just physical; emotional closeness often deepens when you both face adversity together.