When a patient is prescribed a medication, they expect to get exactly what their doctor ordered. But in hospitals and nursing homes, that’s not always what happens. Behind the scenes, a system called an institutional formulary decides whether a drug can be swapped out for another - even if it’s chemically different. This isn’t about pharmacies filling prescriptions. It’s about hospitals and clinics making controlled changes to medication plans to save money, reduce errors, and improve outcomes. And in places like Florida, it’s the law.
What Exactly Is an Institutional Formulary?
An institutional formulary is a living list of approved drugs that a hospital, clinic, or long-term care facility uses as its standard. It doesn’t just say which drugs are available - it tells staff when and how to swap one drug for another that works the same way. This is called therapeutic substitution. For example, if a patient is on brand-name Xarelto, the formulary might allow switching them to apixaban - a different drug, but with similar effects for preventing blood clots. Unlike insurance formularies that decide what drugs a plan will pay for, institutional formularies are about what happens inside the facility. They’re managed by a team of doctors, pharmacists, and nurses who review evidence, cost, and safety before approving any drug. The goal? To make sure patients get effective treatment without unnecessary expense or risk. In Florida, this isn’t optional. Under Statute 400.143 (2025), every nursing home and long-term care facility must have a formal formulary. The law requires a committee with a medical director, nursing director, and a certified pharmacist to create, monitor, and update it. That committee has to write down how decisions are made, notify prescribers when substitutions happen, and check in every three months to see if those changes are helping or hurting patients.How Formularies Decide Which Drugs to Use
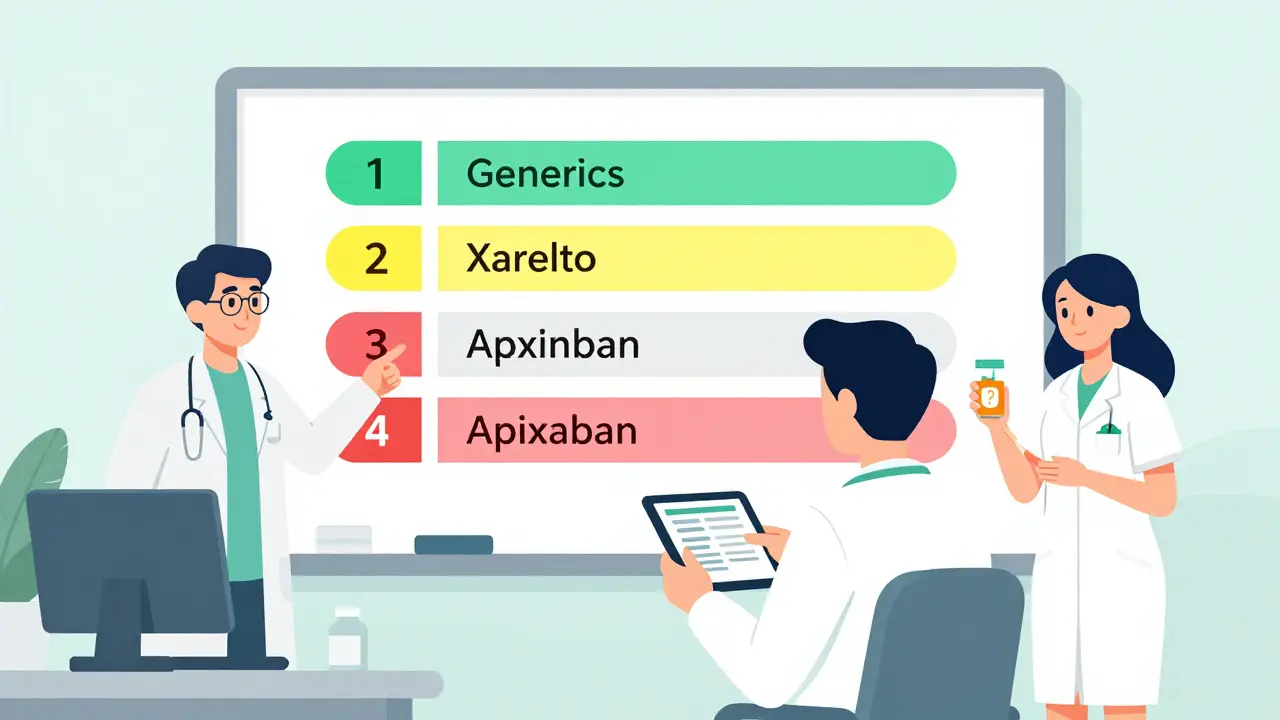
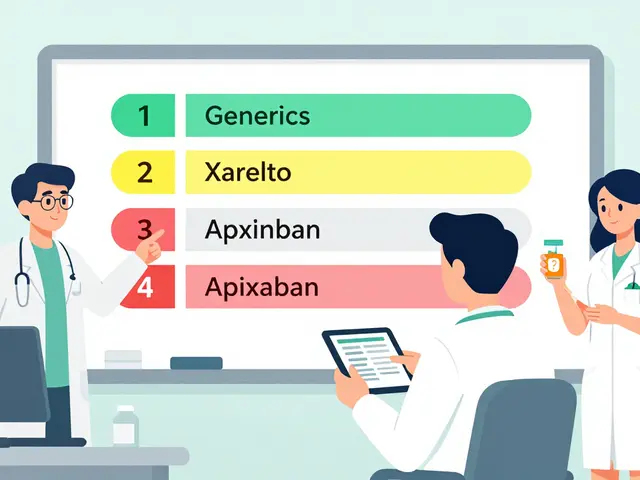
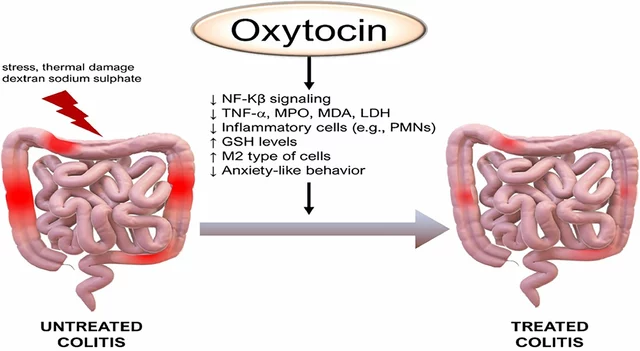
Formularies don’t pick drugs randomly. They use a tiered system, like a ranking ladder. Tier 1 includes the most cost-effective, evidence-backed options - usually generics. These have the lowest cost to the patient and are the first choice. Tier 2 might include brand-name drugs that are slightly more expensive but still proven. Tier 3? That’s where the expensive, niche, or newer drugs go - often requiring special approval to use. The decision process is strict. A panel reviews clinical studies, real-world outcomes, and price data. They ask: Does this drug actually work better than the cheaper alternative? Is it safer? Does it reduce hospital readmissions? A 2018 study in the American Journal of Health-System Pharmacy found that hospitals using strong formularies saw a 15-30% drop in adverse drug events. That’s not just savings - it’s lives saved. But it’s not just about cost. A drug might be cheaper, but if it causes more side effects in elderly patients - common in nursing homes - it won’t make the list. Formularies are designed to balance safety, effectiveness, and affordability. That’s why a drug like metformin, which has decades of safety data and costs pennies, is almost always in Tier 1. Meanwhile, a new $1,200-a-month diabetes drug might be excluded unless it clearly outperforms older options.The Legal Framework: Florida’s Model
Florida’s law, Statute 400.143, is one of the most detailed in the U.S. It doesn’t just say “have a formulary.” It spells out exactly who must be involved, what they must do, and how often they must report results. The committee must:- Define clear criteria for adding or removing drugs
- Write policies for notifying doctors when a substitution happens
- Track clinical outcomes every quarter - like how many patients had falls, infections, or ER visits after a drug change
- Keep all documents ready for state inspectors

Where Formularies Work Best - and Where They Struggle
Institutional formularies shine in long-term care. Patients stay for months or years. Their meds don’t change often. That makes it easier to standardize, monitor, and adjust. In fact, 94% of nursing homes in the U.S. have formal formularies, according to the American Society of Health-System Pharmacists. But in busy emergency rooms or acute care units? It’s trickier. A patient comes in with a sudden heart attack. They’re on a specific blood thinner. The formulary says to switch to a cheaper alternative - but the patient’s condition is unstable. Waiting for approval could delay care. Many hospitals use “exceptions” for these cases, but that adds paperwork and confusion. Worse, when patients move between facilities - say, from a nursing home to a hospital - their meds might get switched back and forth. One Reddit user, a hospital pharmacist, shared a case where a patient was switched from Xarelto to apixaban in a nursing home, then switched back to Xarelto upon hospital admission. No one told the patient or the family. The patient was confused. The family was angry. The risk of error went up. This is a real problem. A 2023 AMA survey found that 78% of physicians worry about bureaucratic delays when trying to get non-formulary drugs for complex patients. A cancer patient on a targeted therapy might need a drug not on the formulary. Getting approval can take days. In some cases, it’s too late.Who’s Involved - And What They Think
It’s not just pharmacists running this show. It’s a team. - Pharmacists are the backbone. They review drug interactions, monitor adherence, and flag unsafe substitutions. In Florida, they must be certified under section 465.0125 - a specific credential that ensures they know the rules. - Doctors often resist. They’re trained to prescribe based on individual needs, not system-wide policies. But many support formularies when they’re evidence-based. The same AMA survey showed 62% of physicians believe formularies improve safety. - Nurses are on the front lines. They give the meds. If a patient’s pill looks different, they’re the ones who notice. Training them to recognize substitutions and explain them to patients is critical. One facility in Orlando reported it took six weeks for nurses to fully adapt to the new system. - Patients and families are often left out. AARP’s Policy Institute pointed out that many long-term care patients don’t even know their meds have been changed. No informed consent. No discussion. That’s a gap. Experts like Dr. Jerry Avorn from Harvard say formularies bring market logic to healthcare - encouraging competition among drug makers and rewarding value. But Dr. Aaron Kesselheim warns: “Restrictions can block access to what patients truly need.” The trick is balance.Implementation Challenges and Fixes
Setting up a formulary sounds simple. But in practice? It’s messy. Most facilities struggle with:- Electronic health record (EHR) integration - 68% of Florida facilities had tech issues when launching their systems
- Staff training - nurses and aides need to understand not just the rules, but why they matter
- Documentation - writing and updating policies takes 20-30 hours per quarter
The Bigger Picture: Costs, Trends, and the Future
Institutional formularies are part of a $600 billion U.S. drug system. About 89% of all prescriptions in the country are affected by some kind of formulary. In nursing homes, that number hits 27% of all prescriptions. Trends are pushing formularies further:- Medicare’s Nursing Home Compare ratings will start factoring in formulary compliance in Q3 2025. Facilities that don’t follow the rules could lose funding.
- By 2026, Gartner predicts 80% of healthcare systems will use AI to adjust formularies in real time based on patient outcomes.
- 72% of healthcare leaders say they’ll start using genetic data to tailor formulary choices within five years - like avoiding a drug if a patient’s genes make them prone to side effects.
What Patients and Families Should Know
If you or a loved one is in a hospital or nursing home, here’s what to ask:- “Is this medication the same as what my doctor prescribed?”
- “Why was it changed?”
- “Can I get the original drug if I prefer it?”
- “Will this change affect how the drug works for me?”
Is This System Working?
Yes - but imperfectly. Institutional formularies have cut drug errors, lowered costs, and improved consistency in care. They’ve turned guesswork into science. But they’re only as good as the people running them. If the committee is overloaded, if doctors feel silenced, if patients are kept in the dark - the system fails. The future of institutional formularies isn’t about more rules. It’s about smarter rules. Rules that adapt to real patients, not just data points. Rules that respect individual needs while still protecting the system. That’s the balance we’re still learning to strike.3 Comments
Naomi Walsh
February 3, 2026 AT 07:53 AM
Oh please. You’re acting like this is some sinister corporate plot. The fact that you’re shocked that hospitals prioritize safety and cost-effectiveness is honestly laughable. Every single drug on a formulary is vetted by a multidisciplinary team-pharmacists, clinicians, nurses-none of whom are profit-driven automatons. The real scandal is how many physicians still treat patients like their personal clinical trials. If a $1,200/month drug doesn’t outperform metformin in real-world outcomes, it shouldn’t be the default. Stop romanticizing brand-name prescriptions as some sacred right. This isn’t capitalism-it’s responsible medicine.
Bryan Coleman
February 3, 2026 AT 17:11 PM
Been working ER and med-surg for 14 years. Formularies? They save lives when done right. But the EHR integration nightmares? Yeah. We had one where the system auto-subbed lisinopril for enalapril and didn’t flag the patient’s history of angioedema. Took three days to catch it. Training matters more than policy. Also, nurses are the ones catching these slips-give ‘em credit. And yeah, patients need to be told when their meds change. Simple as that. No jargon. Just: ‘Your pill looks different because we switched to a cheaper one that works the same.’


Lilliana Lowe
February 1, 2026 AT 13:35 PM
The institutional formulary model, particularly as codified in Florida’s Statute 400.143, represents a paradigmatic shift in pharmacoeconomic governance-elevating evidence-based therapeutics above physician autonomy, which, while noble in intent, often disregards the nuanced pharmacokinetics of individual patients. The reliance on tiered formularies, while statistically defensible, risks reducing clinical decision-making to a spreadsheet algorithm. A 2018 AJHP study cited here is compelling, but meta-analyses from JAMA Internal Medicine (2021) reveal that therapeutic substitution in elderly populations increases non-adherence by 19%-a metric conspicuously absent from the article’s ‘lives saved’ rhetoric. This isn’t cost containment; it’s pharmaceutical rationing dressed in clinical jargon.