DRESS Diagnosis: What It Is, How It’s Identified, and What You Need to Know
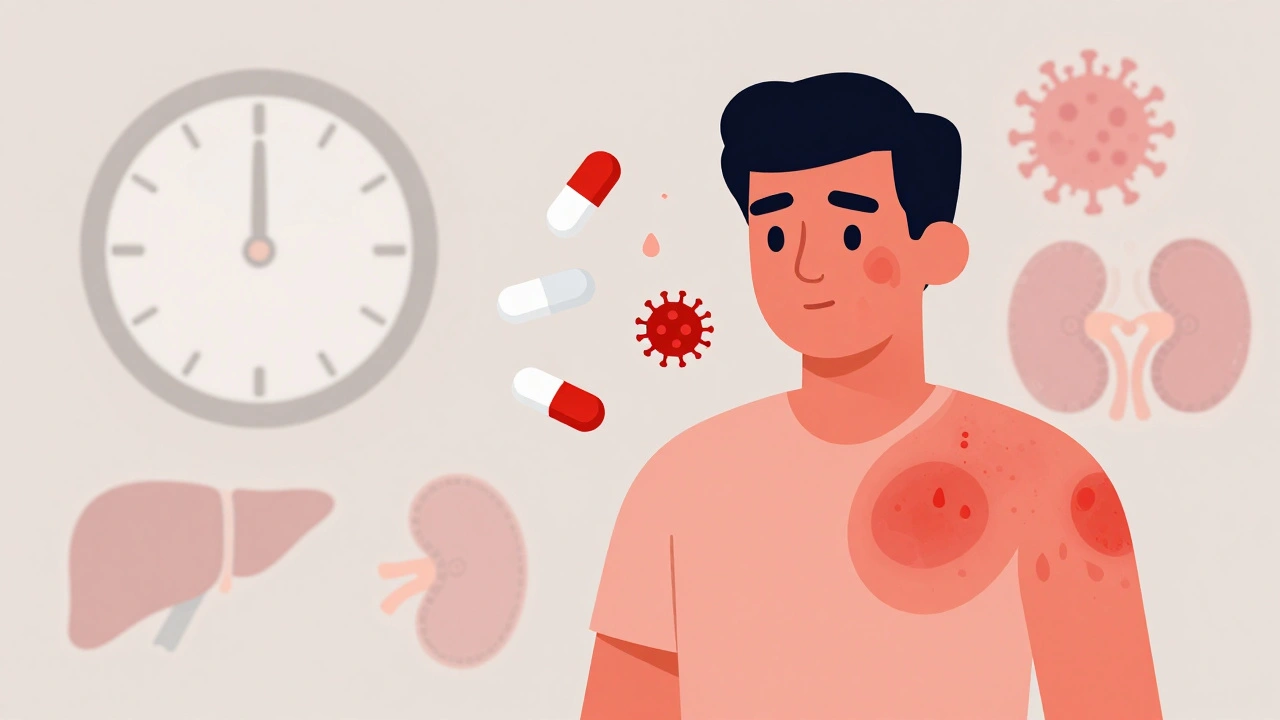
When your body overreacts to a medication, it doesn’t always mean a simple rash or upset stomach. DRESS diagnosis, a severe, delayed drug reaction that affects multiple organs and can be life-threatening. Also known as drug reaction with eosinophilia and systemic symptoms, it’s not just a skin problem—it’s a full-body alarm. Unlike common allergies that show up right after taking a pill, DRESS can take weeks to develop, making it easy to miss or misdiagnose as the flu, hepatitis, or even mononucleosis.
DRESS diagnosis usually shows up after starting a new medication—often anticonvulsants like carbamazepine or phenytoin, antibiotics like sulfonamides, or allopurinol for gout. It brings a mix of symptoms: a widespread rash, swollen lymph nodes, fever, and internal organ involvement like liver or kidney damage. Blood tests often show high eosinophils, a type of white blood cell that spikes in allergic responses. The key to survival? Catching it early. Once the drug is stopped and treatment starts, recovery can take weeks or months. But if ignored, DRESS can lead to organ failure or even death.
Doctors don’t have one single test for DRESS diagnosis. They piece it together using clinical signs, lab results, and a detailed drug history. The RegiSCAR criteria, used by specialists worldwide, help standardize the diagnosis by scoring symptoms like fever, rash, organ involvement, and blood changes. It’s not just about the rash—it’s about the pattern. If you’ve been on a new medication for 2 to 8 weeks and suddenly feel awful with a rash and swollen glands, ask your doctor: Could this be DRESS?
What makes DRESS diagnosis tricky is that it looks like so many other things. It’s often mistaken for viral infections because of the fever and fatigue. Or it’s written off as a side effect when the real issue is a dangerous immune overreaction. Even experienced clinicians can delay the right call—especially if the patient doesn’t mention every pill they’ve taken, including over-the-counter drugs or herbal supplements.
Some people are genetically at higher risk. For example, those with the HLA-B*58:01 gene variant have a much higher chance of developing DRESS from allopurinol. That’s why in some countries, doctors test for this gene before prescribing the drug. It’s not routine everywhere, but it should be—especially if you’re Asian or have a history of severe drug reactions.
Once DRESS diagnosis is confirmed, the first step is stopping the offending drug—no exceptions. Steroids are often needed to calm the immune system, and hospitalization is common. Recovery isn’t quick. Some people get better in weeks. Others deal with long-term organ damage or develop autoimmune conditions later. And here’s the catch: once you’ve had DRESS from one drug, you’re at higher risk for it with others in the same class. That’s why keeping a detailed drug allergy list matters—every time you see a new doctor.
Below, you’ll find real-world posts that dig into how drug reactions happen, how to spot hidden dangers in common meds, and what to do when your body says no. From how antibiotics trigger immune chaos to why even expired pills can cause unexpected harm, these articles give you the tools to recognize red flags before they become emergencies. You won’t find fluff here—just clear, practical info to help you stay safe when taking medication.
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS): What You Need to Know Now
DRESS syndrome is a rare but deadly drug reaction that strikes weeks after taking certain medications. Learn the signs, triggers, and how to get diagnosed before it’s too late.
View More




