Drug Hypersensitivity: What It Is, How It Happens, and What to Do
When your body treats a medication like a threat, that’s drug hypersensitivity, an immune system overreaction to a medicine that isn’t toxic at normal doses. Also known as medication allergy, it’s not the same as a side effect—like dizziness or nausea—that everyone might get. This is your immune system sounding the alarm, even when the drug is perfectly safe for most people. It can show up as a simple itch, or it can shut down your breathing in minutes. That’s why understanding it isn’t just helpful—it’s critical.
One of the most serious forms is anaphylaxis, a rapid, whole-body allergic reaction that can be fatal without immediate treatment. Also known as severe allergic reaction, it’s often triggered by antibiotics, NSAIDs, or contrast dyes used in imaging. If you’ve ever had swelling in your throat, a sudden drop in blood pressure, or hives after taking a pill, you’ve seen this in action. And it’s not rare: studies show nearly 5% of hospital visits for drug reactions are due to hypersensitivity. The scary part? You might not know you’re at risk until it happens.
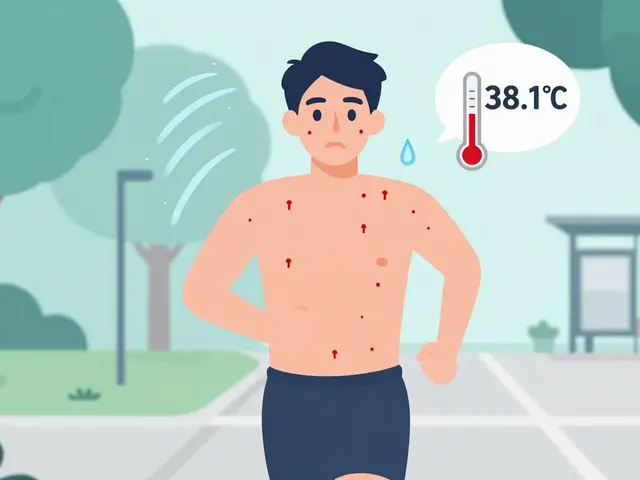
Not all reactions are dramatic. Some show up days later as a rash, fever, or joint pain—this is called a delayed hypersensitivity, a slower immune response that’s harder to link to the drug causing it. These are often missed because they don’t happen right after you take the medicine. Doctors may think it’s a virus or an unrelated condition. But if you’ve had a reaction before, even a mild one, that’s your body’s warning. It’s not just "bad luck." It’s a signal.
What makes this even trickier is that some drugs cause reactions across entire classes. If you’re allergic to penicillin, you might also react to amoxicillin—even if you’ve taken it before without issues. That’s why knowing the difference between a drug-specific reaction and a class-wide one matters. One wrong pill could cost you more than discomfort—it could cost you your life.
And it’s not just about the active ingredient. Sometimes, the fillers or dyes in generics trigger reactions too. You might think you’re safe because you’ve taken "the same drug" before—but if the brand changed, the inactive ingredients might not be. That’s why checking every pill you take isn’t paranoia—it’s smart.
So what do you do? Keep a list. Write down every medication you’ve reacted to, what happened, and when. Show it to every doctor, pharmacist, and ER nurse. Don’t say "I’m allergic to antibiotics"—say "I broke out in hives after amoxicillin." Specifics save lives. And if you’ve ever had trouble breathing after a shot or pill, carry an epinephrine auto-injector. It’s not just for peanuts.
Below, you’ll find real stories and science-backed advice on how to recognize, avoid, and respond to these reactions. From how to tell if a warning applies to your whole drug class to what to do when your body says no—this isn’t theory. It’s what people actually need to survive.
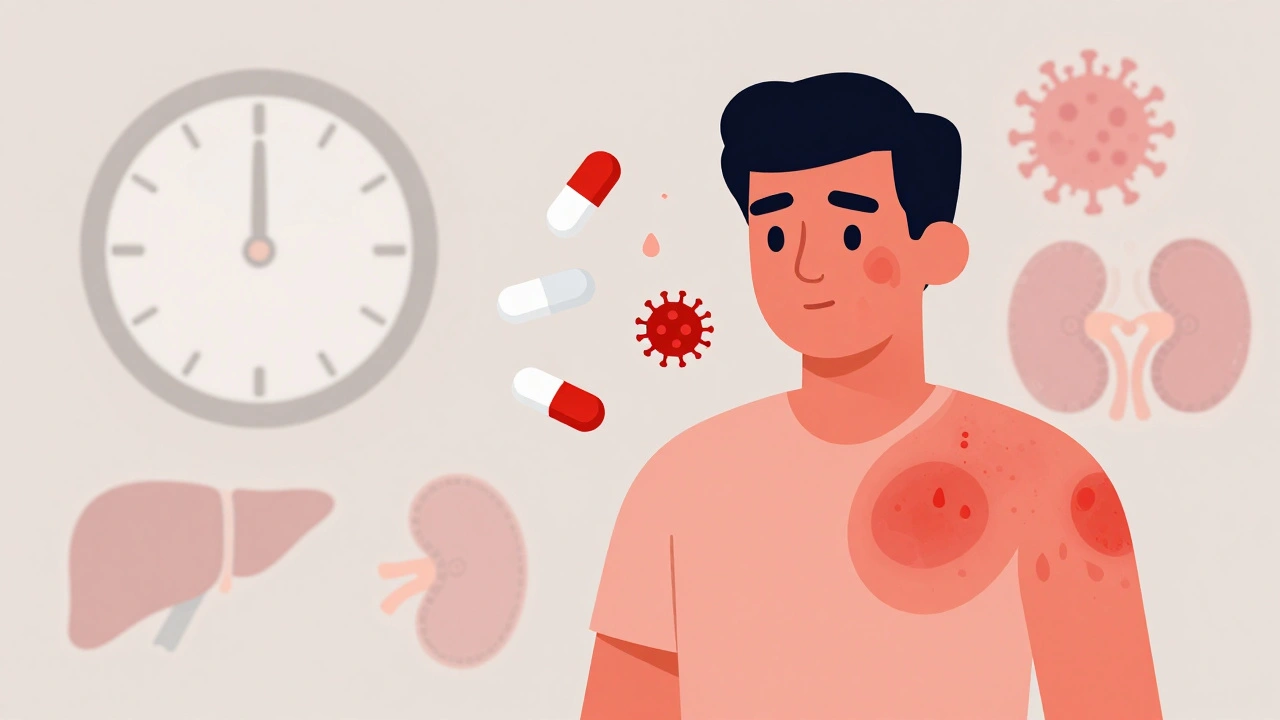
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS): What You Need to Know Now
DRESS syndrome is a rare but deadly drug reaction that strikes weeks after taking certain medications. Learn the signs, triggers, and how to get diagnosed before it’s too late.
View More