Imagine breaking out in tiny, itchy bumps just after you start jogging, walking to the bus, or even eating a spicy meal. No allergens. No new soap. No bee sting. Just heat. That’s cholinergic urticaria - a condition where your body overreacts to its own sweat, turning normal temperature rises into a full-blown skin storm.
What Exactly Is Cholinergic Urticaria?
Cholinergic urticaria (CU) isn’t just a heat rash. It’s an immune system glitch triggered by a rise in core body temperature. When you sweat - whether from exercise, hot weather, stress, or even a hot shower - nerve fibers around your sweat glands send the wrong signal. Mast cells in your skin respond by dumping histamine, and that’s when the hives appear.
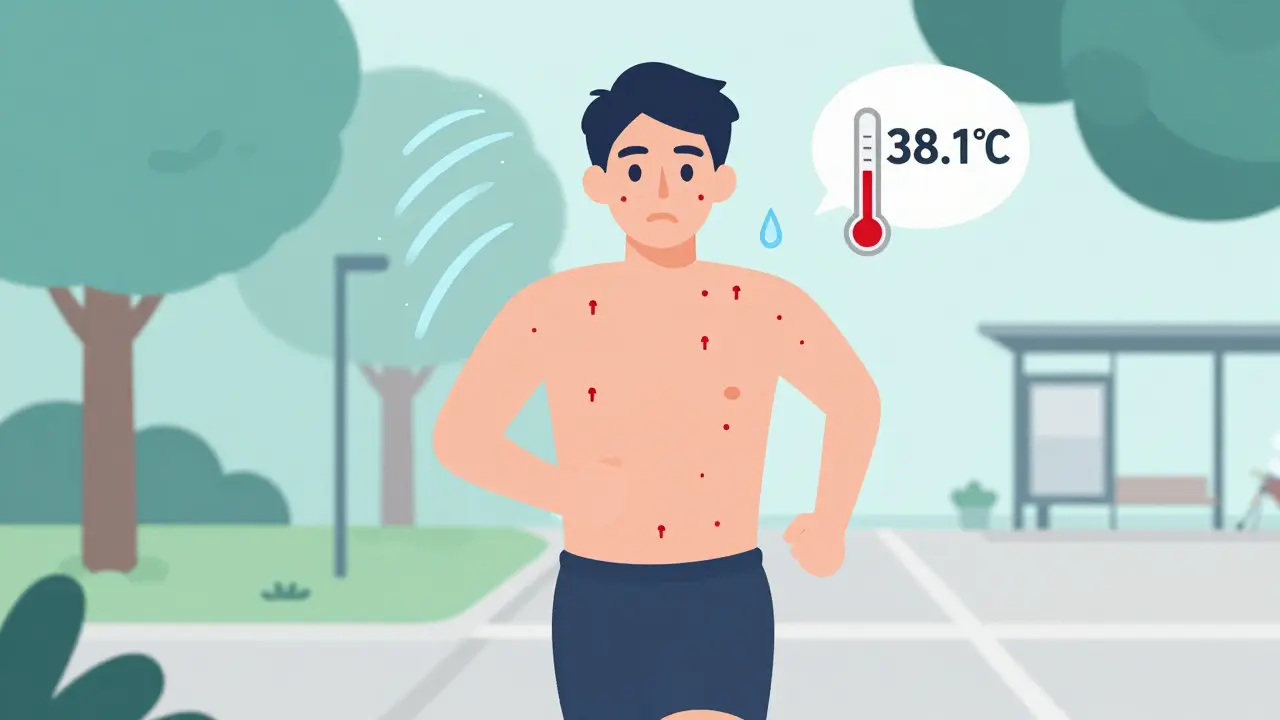
These aren’t big, angry welts like allergic reactions. They’re small - about 1 to 3 millimeters - like pinpricks surrounded by red flares. You’ll feel them before you see them: a prickling, tingling warmth that spreads fast across your chest, neck, face, and upper back. The skin feels hot to the touch, even if the room is cool.
It hits fast. Within 2 to 15 minutes of getting warm, the bumps show up. They don’t last long - usually 15 to 30 minutes - and fade completely within 90 minutes once you cool down. But that short window is enough to ruin a workout, a date, or a family dinner.
Who Gets It and Why?
Most people first notice cholinergic urticaria between ages 15 and 25. It’s rare in kids under 10 and uncommon after 50. Men and women are affected equally, but it’s more common in people with a history of other allergies or asthma.
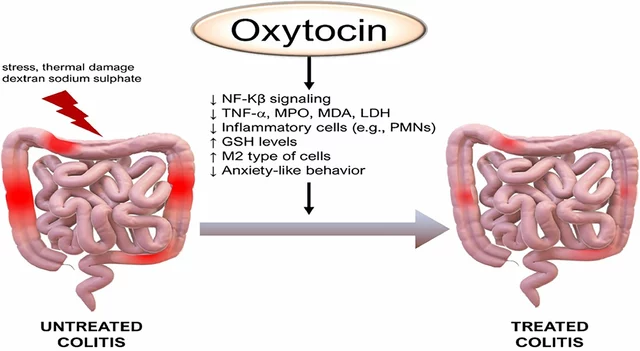
Why does this happen? Research shows it’s not about being allergic to sweat. It’s about how your skin’s nerves and immune cells talk to each other. People with CU have lower levels of acetylcholinesterase - the enzyme that normally breaks down the chemical acetylcholine - in their sweat glands. That means acetylcholine builds up, overstimulating receptors on mast cells, which then release histamine like a fire alarm gone wild.
It’s also linked to higher levels of certain immune signals - CCL2, CCL5, CCL17 - that pull in T-cells to the skin. That’s why the reaction is localized but intense. It’s not an allergy to food or pollen. It’s your own body misfiring under heat stress.
What Triggers It? Beyond Just Exercise
Most people think exercise is the main trigger - and they’re right. About 9 in 10 patients report flare-ups during or after physical activity. But it’s not just the gym.
- Spicy food: Capsaicin in chili peppers tricks your body into thinking it’s overheating. One survey found 67% of CU patients get hives after eating hot meals.
- Hot showers or baths: Even a 10-minute hot shower can be enough to trigger a reaction.
- Emotional stress: Anxiety or nervousness raises your core temperature. Many report outbreaks before presentations, interviews, or public speaking.
- Humid weather: When sweat can’t evaporate, your body keeps heating up. That’s why CU is more common in Southeast Asia than Scandinavia.
- Tight clothing: Fabric that traps heat and moisture - like polyester workout gear - makes it worse.
What doesn’t trigger it? Cold, sunlight, pressure from a backpack, or rubbing your skin. That’s how you tell CU apart from other types of hives.

How Is It Diagnosed?
Doctors don’t guess. They test. The gold standard is the passive warming test. You sit in a warm room (around 39°C) while your core temperature is monitored. A small increase - just 0.5°C above your normal 37°C - is enough to trigger the classic 1-3mm hives in 94% of people with CU.
Some clinics use exercise tests - riding a stationary bike until you sweat - but that’s less controlled. The passive test is safer and more accurate.
Many patients are misdiagnosed. About 22% of people who go to the ER with heat-triggered hives are told they’re having exercise-induced anaphylaxis. But CU rarely causes breathing trouble or low blood pressure - unless it’s severe.
How Bad Can It Get?
For most people, CU is annoying. For some, it’s dangerous.
While the hives themselves are uncomfortable, 12.3% of patients report systemic symptoms: dizziness, rapid heartbeat, wheezing, or even a drop in blood pressure. In 8.7% of cases, doctors recommend carrying an epinephrine auto-injector - not because it’s common, but because the risk is real.
One Reddit user wrote: “I missed 14 weddings in three years because I can’t risk overheating in formal attire.” That’s the hidden cost. It’s not just skin deep. It affects relationships, jobs, travel, and mental health. Studies show 62% of CU patients report moderate to severe impact on quality of life - higher than eczema or rosacea.
What Treatments Actually Work?
There’s no cure. But there are ways to take back control.
First-line treatment: Non-sedating antihistamines. Cetirizine (Zyrtec) or loratadine (Claritin) at standard doses (10mg daily) help about 68% of people. If that’s not enough, doctors often increase the dose - up to 40mg of cetirizine daily. That’s four times the usual amount, and it’s safe under medical supervision.
Second-line: Adding an H2 blocker. If antihistamines alone aren’t cutting it, adding famotidine (Pepcid) 20mg twice a day helps 57% of resistant cases. It blocks a different histamine receptor, giving you a second line of defense.
For severe, stubborn cases: Omalizumab (Xolair). Approved in Europe in 2023 for CU, this injectable biologic targets IgE antibodies. In trials, 78% of patients saw their hives disappear completely with weekly shots. But it’s expensive - around $3,500 per month in the U.S. - and not widely used yet.
First-generation antihistamines like diphenhydramine (Benadryl) are avoided. They cause drowsiness, and 58% of users say it messes with their work or driving. You need to stay alert. You don’t need to be asleep.

Prevention: The Real Game-Changer
Medication helps. But prevention? That’s where you regain your life.
- Know your trigger temperature. Most CU patients hit their limit around 38.1°C core temperature. Use a wearable thermometer or pay attention to how you feel. That warm flush? That’s your warning.
- Wear moisture-wicking clothes. Cotton traps sweat. Synthetic blends like polyester or merino wool pull it away. Look for labels that say “cooling” or “performance fabric.”
- Train smart. Do workouts in air-conditioned spaces. Use fans. Take breaks every 10 minutes. Cool your wrists and neck with a damp cloth. One patient cut flare-ups from daily to 1-2 times a month just by switching to indoor workouts.
- Avoid spicy foods before activity. If you know chili triggers you, skip the hot sauce before a run.
- Pre-cool before exertion. Drink a cold beverage. Wet your shirt. Sit in front of a fan for 10 minutes before you start moving.
- Use a tracking app. The Urticaria Center of Excellence’s free app lets you log temperature, activity, food, and symptoms. Users report 85% satisfaction. It helps you spot patterns you’d never notice.
What Doesn’t Work - And Why
Some advice you’ll hear is misleading:
- “Just avoid sweating.” Impossible. You sweat when you’re nervous, eating, sleeping, or walking in summer. You can’t live in a fridge.
- “Try natural remedies.” No evidence that quercetin, vitamin C, or nettle tea helps CU. They might help other allergies, but not this one.
- “Take antihistamines before every activity.” You’ll build tolerance. And constant use can cause side effects. Use them strategically - not as a crutch.
The Future: What’s Coming Next?
Research is moving fast. By 2026, doctors hope to have two reliable biomarkers to diagnose CU with a blood test - no warming test needed.
Wearable tech is catching up. ThermaCare and Mayo Clinic are testing smart shirts that monitor skin temperature and vibrate when you’re about to overheat. Early tests show a 63% drop in flare-ups.
And then there’s climate change. As global temperatures rise, CU could become more common - especially in temperate zones. One study predicts a 15-25% increase in cases by 2040.
For now, the best tool you have is knowledge. Know your triggers. Track your body. Talk to a dermatologist who’s seen this before. You’re not imagining it. And you’re not alone.
Can cholinergic urticaria go away on its own?
Yes, about 30% of people see their symptoms fade completely within 7 to 10 years. It’s more likely if you’re under 30 when it starts. But for many, it’s a long-term condition that improves with age and better management - not because it disappears, but because you learn how to control it.
Is cholinergic urticaria dangerous?
Most of the time, no. The hives are uncomfortable but not life-threatening. But in about 1 in 8 cases, people develop systemic symptoms like dizziness, wheezing, or low blood pressure. If you’ve ever felt your throat closing or your heart racing during a flare-up, you should carry an epinephrine auto-injector. Talk to your doctor about your risk level.
Can I still exercise with cholinergic urticaria?
Absolutely - but you need to change how you do it. Work out in cool environments. Use fans or air conditioning. Take frequent breaks. Start slow. Many people find that with the right prep - cooling down first, wearing the right clothes, and taking antihistamines - they can stay active without flare-ups. Some even train their bodies to tolerate heat better over time.
Why do I get hives after a hot shower?
Hot water raises your core body temperature, even if you’re not sweating yet. Your skin heats up, sweat glands activate, and your body triggers the same immune response as exercise. Try lowering the water temperature to lukewarm. Or, take a cool-down shower after the hot one to reset your skin’s response.
Are there any foods I should avoid?
Spicy foods are the biggest dietary trigger - chili peppers, hot sauce, curry, wasabi. Alcohol can also raise your body temperature and dilate blood vessels, making hives worse. Caffeine? Less clear, but some people report more flare-ups after coffee. Keep a food diary for 2 weeks. You might be surprised what sets you off.
Should I see a specialist?
Yes - a dermatologist or allergist who specializes in physical urticaria. General practitioners often don’t recognize CU and may misdiagnose it as stress rash or heat exhaustion. A specialist can run the passive warming test, rule out other conditions, and help you build a personalized plan - including whether you need an epinephrine pen or higher-dose meds.
5 Comments
Suresh Kumar Govindan
January 25, 2026 AT 09:21 AM
One must question the underlying pathophysiological paradigm. The autonomic dysregulation hypothesis fails to account for epigenetic modulation of cholinergic receptors in dermal mast cells. Peer-reviewed literature remains insufficiently rigorous.
TONY ADAMS
January 25, 2026 AT 12:29 PM
bro i got hives after eating a burrito and thought i was dying. turned out it was this. i just chill now and avoid spicy stuff. no more gym for me lol.
Josh josh
January 26, 2026 AT 22:58 PM
heat hives got me missing my cousin's wedding in july. i sat in the car with the ac on full blast while everyone danced. no regrets. just wear cotton and chill
also i got a smart shirt last year and it beeped when i was getting too warm. saved my life literally
Rakesh Kakkad
January 28, 2026 AT 08:19 AM
It is imperative to acknowledge the role of environmental humidity in exacerbating the condition. In tropical climates, the evaporation rate of sweat is significantly reduced, thereby amplifying the thermoregulatory response. This phenomenon is not adequately addressed in Western medical literature.




Nicholas Miter
January 25, 2026 AT 01:05 AM
Been dealing with this for years. I used to think I was just bad at exercising until I realized it wasn't the effort-it was the sweat. Now I keep a mini fan in my gym bag and it's a game changer.
Also, lukewarm showers. No more scalding. Life's better this way.