IBS Treatment: Effective Ways to Manage Symptoms and Find Relief
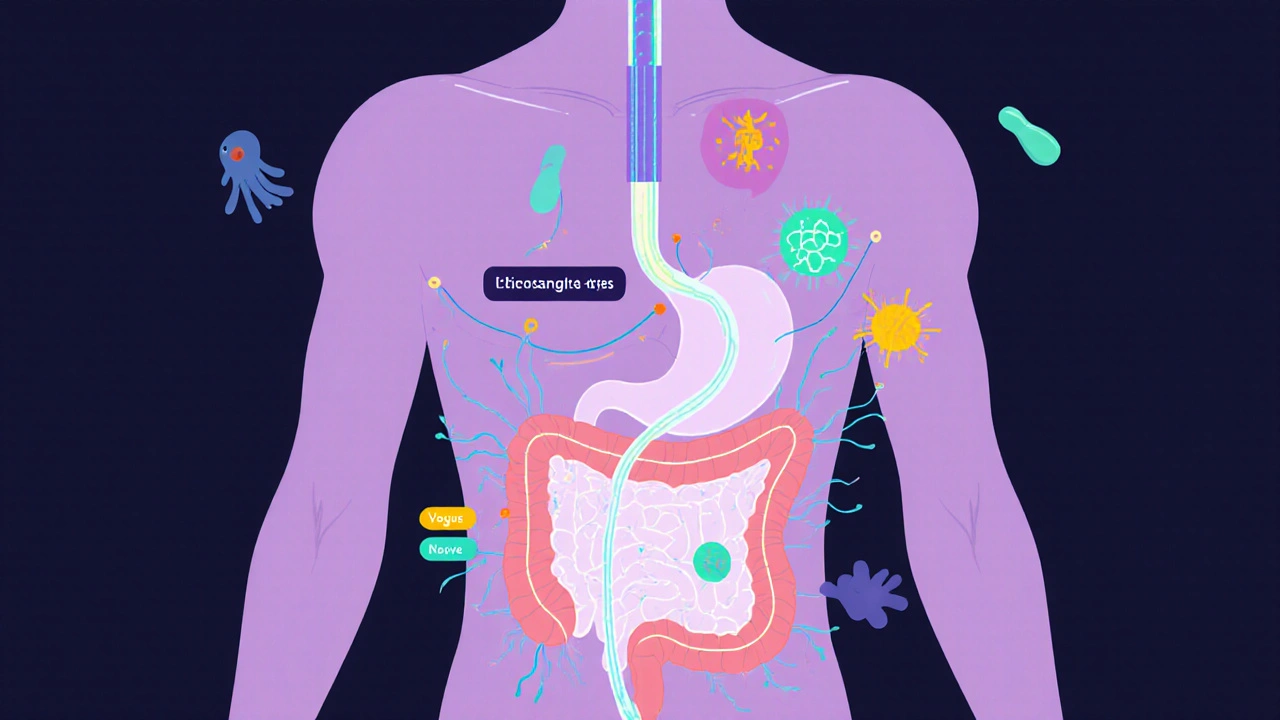
When you have irritable bowel syndrome, a common digestive disorder that causes cramping, bloating, diarrhea, and constipation without visible damage to the gut. Also known as spastic colon, it doesn’t show up on scans or blood tests—but the pain is real, and it can wreck your daily life. Millions live with it, often told it’s "just stress" or "all in your head." But IBS isn’t imagination. It’s a brain-gut connection gone wrong, where nerves in your intestines become oversensitive and react strongly to food, stress, or even normal digestion.
Managing IBS treatment isn’t about one magic pill. It’s about matching your triggers to your body. Some people flare up after dairy, others after gluten, coffee, or artificial sweeteners. The low FODMAP diet isn’t a fad—it’s backed by studies showing up to 70% of people get better when they cut out certain fermentable carbs. But it’s not a lifelong sentence. Most people reintroduce foods slowly to find their personal tolerance. Then there’s stress—your gut has more nerves than your spine. When you’re anxious, your digestive system slows, spasms, or races. Simple breathing exercises, therapy, or even daily walks can calm the signal between your brain and bowels.
Medications play a role too. Antispasmodics like dicyclomine can ease cramps. Laxatives or anti-diarrheals help balance bowel habits. For some, low-dose antidepressants like amitriptyline calm nerve pain in the gut—not because they’re depressed, but because they change how pain signals travel. And probiotics? Not all are equal. Certain strains like Bifidobacterium infantis have shown real results in clinical trials. But skip the generic store brands—look for ones backed by research.
What you won’t find in most IBS guides? The truth about how antibiotics, birth control, or even sleep quality can trigger flares. Or how food intolerances can mimic IBS but need completely different fixes. Or why some people feel better with peppermint oil capsules, while others get worse. This collection of posts doesn’t just list treatments—it shows you what actually works, what’s overhyped, and what to watch out for when your symptoms change.
Below, you’ll find real stories and science-backed advice from people who’ve been there—from how to track your triggers without obsession, to what to do when standard advice fails, to how to talk to your doctor without sounding like you’re just looking for a quick fix. No fluff. No guesswork. Just what helps, what doesn’t, and why.
Irritable Bowel Syndrome: Understanding the Gut-Brain Axis for Real Symptom Relief
Irritable Bowel Syndrome isn't just digestive trouble-it's a breakdown in gut-brain communication. Learn how stress, microbes, and nerve signals drive symptoms, and what actually works to restore balance and find lasting relief.
View More




