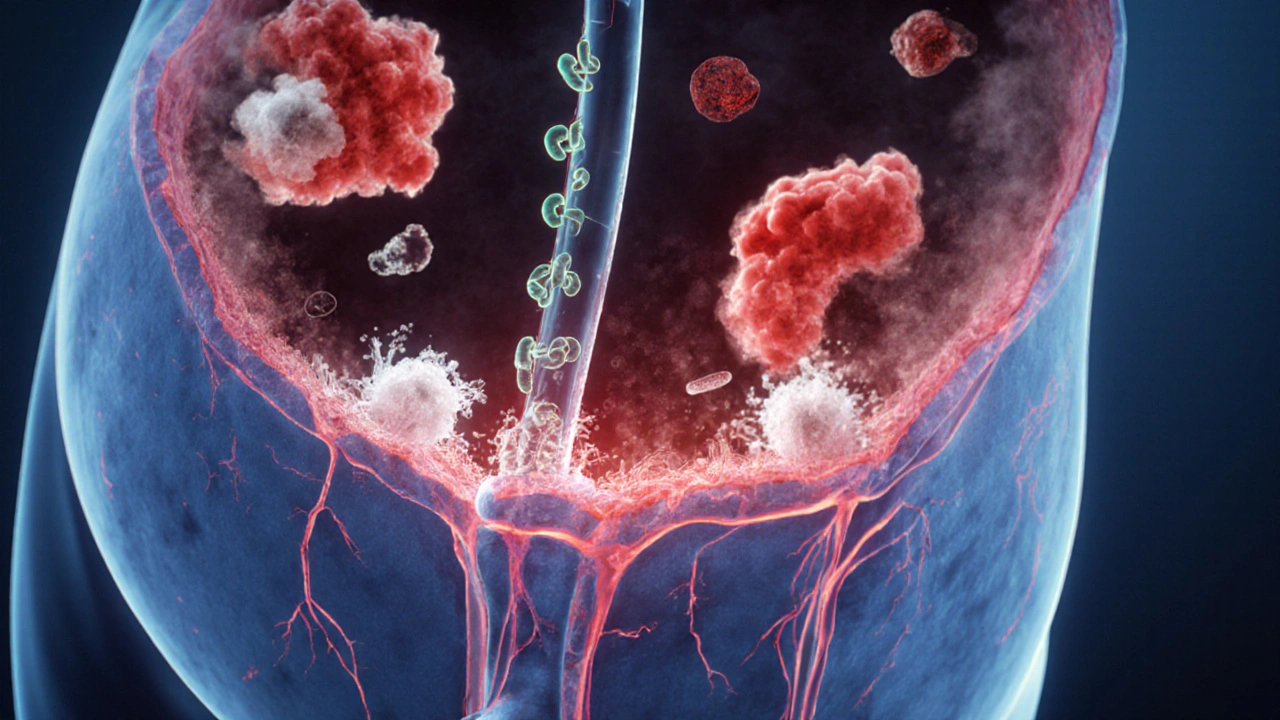
Urinary Tract Infection (UTI) Overview
When dealing with urinary tract infection, a bacterial invasion of the urinary system that causes painful urination and frequent urges. Also known as UTI, it commonly affects the bladder and can spread to the kidneys. Prompt treatment with antibiotics is essential to prevent complications.
A urinary tract infection is not just a single disease; it’s a spectrum that includes cystitis (bladder infection), urethritis, and pyelonephritis (kidney infection). Each stage has its own set of symptoms: burning during urination, cloudy or foul‑smelling urine, lower‑abdominal pain for cystitis, and fever, flank pain, or chills when the kidneys are involved. Recognizing these signs early lets you act fast, because the longer the bacteria linger, the higher the chance of kidney damage or recurrent episodes.
Why do some people get UTIs repeatedly while others never do? The answer lies in a mix of anatomy, hygiene habits, and underlying health conditions. Women are more prone because of a shorter urethra, and factors like sexual activity, contraceptive devices, or menopause can shift the balance of normal flora. Diabetes, urinary catheters, and kidney stones create environments where bacteria thrive. Understanding your personal risk profile helps you make targeted changes, such as staying hydrated, wiping front‑to‑back, and avoiding irritating soaps.
When it comes to treatment, antibiotics are the frontline weapons. Common choices include trimethoprim‑sulfamethoxazole (Bactrim), nitrofurantoin, and fosfomycin. The right drug depends on local resistance patterns, allergy history, and whether the infection is uncomplicated or has reached the kidneys. For uncomplicated cystitis, a three‑day course often suffices, while pyelonephritis may require a longer, sometimes intravenous, regimen. Our post collection includes a detailed look at generic Bactrim buying tips, which can help you save money without compromising safety.
Prevention is just as vital as cure. Simple habits—drinking plenty of water, urinating after intercourse, and avoiding douches or harsh feminine products—can keep bacteria from colonizing the urinary tract. Probiotic‑rich foods and, in some cases, low‑dose cranberry extracts may add a protective layer, though the evidence is mixed. For those with recurrent UTIs, a healthcare provider might suggest a post‑coital antibiotic dose or a low‑dose prophylactic regimen. Our guide on antibiotic comparisons can help you weigh the pros and cons of different options if you ever need a long‑term plan.
Below you’ll find a curated set of articles that dive deeper into each aspect of UTIs— from symptom checklists and when to seek emergency care, to side‑by‑side drug comparisons, buying guides for generic antibiotics, and lifestyle tweaks that lower your risk. Whether you’re looking for a quick answer or a comprehensive plan, the collection is organized to give you actionable insights right away.
UTI and Chronic Fatigue Syndrome: How Infections Trigger Fatigue
Explore how urinary tract infections can trigger chronic fatigue syndrome, the shared biological pathways, evidence, prevention tips, and steps to manage post‑UTI fatigue.
View More




