
Medication Cost-Benefit Calculator
How Expensive Medications Compare
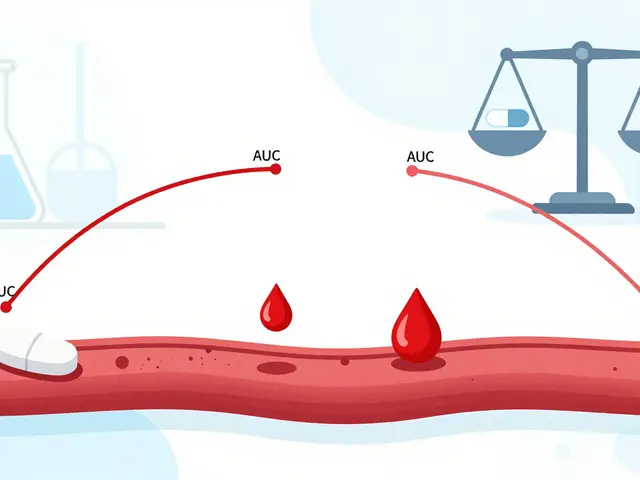
Use this calculator to evaluate if expensive medications provide value based on cost-effectiveness ratios. The calculator shows you how much it costs to gain one quality-adjusted year of life (QALY) for both standard and new treatments.
It’s not hard to understand why a $500,000 cancer treatment makes people pause. That’s more than most families make in a year. But for some, it’s the only shot they have left. When a drug costs more than a new car-and comes with side effects that leave you hospitalized-how do you decide it’s worth it? The answer isn’t about being rich or brave. It’s about cost versus benefit-and what happens when the math doesn’t match the pain.
When the Price Tag Matches the Lifesaving Power
Not all expensive drugs are created equal. Some are just overpriced. Others? They change everything. Take hepatitis C. Ten years ago, treatment meant weekly injections, brutal flu-like symptoms, and a 50% cure rate. Today, a 12-week course of Harvoni can cure 95% of patients with one pill a day. The out-of-pocket cost in 2016? Over $7,000. But compared to the alternative? No more vomiting every day. No more liver failure. No more waiting for a transplant. That’s not just a drug. It’s a reset.Same goes for CAR-T cell therapy. Treatments like tisagenlecleucel cost $475,000 per dose. Patients get cytokine release syndrome-fever, low blood pressure, sometimes ICU stays. But for kids with leukemia who’ve run out of chemo options? This isn’t a gamble. It’s a second chance. A 2023 ASCO patient survey found 78% of families said the side effects were worth it because their child was in remission. No more hospital visits. No more transfusions. Just normal life.
The Hidden Math Behind the Price
Behind every high-cost drug is a number: the incremental cost-effectiveness ratio, or ICER. It’s a fancy way of asking, “How much does it cost to add one more year of healthy life?” In the U.S., anything under $150,000 per quality-adjusted life year (QALY) is generally seen as acceptable. That’s not a law-it’s a guideline. But it’s the number doctors and insurers use to decide if a drug makes sense.Take daratumumab, a multiple myeloma drug. In 2016, NICE in the UK rejected it because its ICER was £120,000 per QALY-way over their £30,000 limit. But after the manufacturer dropped the price, the ICER fell to £45,000. It got approved. That’s the real story: price isn’t fixed. It’s negotiable. And when it drops, the benefit suddenly outweighs the cost.
Meanwhile, 56% of the 50 most expensive drugs in the U.S. were rated as having low or no added benefit by health agencies in France and Germany. That’s not because those countries are cheap. It’s because they demand proof. Not just “it works better,” but “it works better enough to justify the price.”
Side Effects? Maybe They’re Better Than the Alternative
We talk about side effects like they’re the enemy. But sometimes, the side effect is the price of survival. Chemotherapy causes hair loss. Nausea. Fatigue. But if you don’t take it, you die. The same logic applies to newer drugs.Consider emicizumab for hemophilia. It costs $15,000 a month. Patients need infusions every week. But before this drug, they had to get infusions three times a week-each one a needle stick into a vein, often with bleeding complications. Many ended up with permanent joint damage. Now, with emicizumab, they get one shot a week. Fewer bleeds. Fewer hospital trips. Even with the cost and the side effects (headaches, joint pain), patients report better mobility, less pain, and more freedom.
A Reddit thread from June 2023 had a dad write: “My son went from wheelchair to walking again. The side effects? A headache and a sore arm. Worth it.” That’s not emotion. That’s data. That’s quality of life.

Why the U.S. System Is Broken-And How Some Still Win
The U.S. has no national cost-effectiveness threshold. No centralized review. No bargaining power. That means 96% of the most expensive drugs can’t be negotiated under the Inflation Reduction Act. Insurance companies pay list price. Patients pay the rest.Medicare Part D beneficiaries without low-income subsidies spent 2.5 times more out-of-pocket than commercially insured people for these same drugs. One woman skipped doses of ruxolitinib because she couldn’t afford the $5,700 monthly bill. She had polycythemia vera. Her blood thickened. She nearly had a stroke. She didn’t tell her doctor. She just stopped.
But here’s the twist: some people still get access. How? Patient assistance programs. Manufacturer coupons. Foundations like the Chronic Disease Fund gave $2.1 billion in help in 2022. Specialty pharmacies assign case managers who spend over three hours per patient just to get insurance approval. One man with rheumatoid arthritis got his $12,000-a-month drug covered after his case manager fought for 14 days, appealed three denials, and found a nonprofit that covered 70% of his copay.
It’s not fair. But it’s real.
What Makes a Drug Worth It? Three Rules
After reviewing hundreds of cases-from cancer to rare diseases-three patterns stand out:- If it stops a disease from killing you-even if it costs $100,000-it’s often worth it. Think gene therapies for spinal muscular atrophy. One shot. Lifesaving. No more ventilators. No more feeding tubes.
- If it replaces something worse-like switching from daily injections with severe side effects to a monthly pill-it’s worth it. The side effects matter less when the old treatment was worse.
- If it gives you back your life-not just more time, but better time-then the cost becomes secondary. A 62-year-old man with psoriatic arthritis went from unable to hold his granddaughter to hiking with her. His drug cost $14,000 a month. He paid $300 thanks to a foundation. He says: “I’d pay $14,000 again.”

The Real Problem Isn’t the Price-It’s the System
The outrage isn’t about the drug. It’s about the system that lets one company set any price it wants. A drug that costs $20,000 to make gets sold for $500,000. The manufacturer says R&D costs $2.6 billion. But studies show most of that goes to marketing, not science. The FDA approved 50 new drugs between 2017 and 2018. 32 of them offered only minor improvements over existing treatments.Meanwhile, 68% of patients on drugs over $10,000 a month skip doses because they can’t afford them. 42% choose between medicine and food. That’s not a medical decision. That’s a moral failure.
But here’s what’s changing: Medicare is finally starting to negotiate prices in 2024. The first 10 drugs are being targeted-mostly cancer and diabetes drugs that cost billions in public spending. If this works, it could force manufacturers to lower prices across the board.
What You Can Do Right Now
If you or someone you love is facing an expensive drug:- Ask your doctor: “Is there a cheaper alternative with similar results?”
- Call the manufacturer. Almost all have patient assistance programs. You might pay $0.
- Check foundations like the Patient Access Network Foundation, the Chronic Disease Fund, or NeedyMeds. They help people pay.
- Ask your pharmacy for the net price, not the list price. Rebates lower the real cost-but insurers rarely pass it on.
- If you’re on Medicare, ask about the “catastrophic coverage” phase. Once you hit $8,000 out-of-pocket, your copay drops to 5%.
There’s no shame in asking for help. Thousands do it every day.
Final Thought: The Human Equation
A drug isn’t just a number. It’s a child who can run again. A parent who can hug their grandchild. A person who doesn’t have to choose between eating and breathing.The cost of these drugs is high. The side effects are real. But the cost of doing nothing? That’s higher.
Are expensive drugs always worth it?
No. Many high-cost drugs offer only minor improvements over cheaper options. Studies show 32 of 50 new drugs approved between 2017 and 2018 had little to no advantage over existing treatments. The key is whether the drug provides a meaningful improvement in survival or quality of life. If it does, the cost may be justified. If it doesn’t, it’s often overpriced.
Can I get help paying for expensive medications?
Yes. Most drug manufacturers offer patient assistance programs that can cover 40% or more of out-of-pocket costs. Foundations like the Chronic Disease Fund, Patient Access Network Foundation, and NeedyMeds also provide grants. Specialty pharmacies and case managers can help you apply. In 2022, these programs distributed over $2 billion in financial aid.
Why do some countries reject expensive drugs?
Countries like the UK, France, and Germany use formal cost-effectiveness thresholds. The UK’s NICE rejects drugs if they cost more than £30,000 per quality-adjusted life year gained. They don’t say no to treatment-they say no to price tags that don’t match clinical value. This forces manufacturers to negotiate lower prices or prove the drug is truly groundbreaking.
Do side effects make expensive drugs not worth it?
Not always. Side effects matter, but they’re weighed against the disease. For example, CAR-T therapy causes dangerous cytokine storms, but for patients with terminal leukemia, it’s the only option that leads to long-term remission. If the alternative is death or severe disability, many patients accept the risks. The trade-off isn’t just medical-it’s personal.
Is the U.S. system unique in allowing high drug prices?
Yes. Most high-income countries have government agencies that evaluate cost-effectiveness and negotiate prices. The U.S. doesn’t. Medicare couldn’t negotiate prices until 2024, and even then, only 10 drugs are targeted. As a result, Americans pay 2-3 times more for the same drugs than patients in Canada or Germany.
Will drug prices go down in the future?
Possibly. The Inflation Reduction Act’s drug price negotiations are just starting, and early results show manufacturers lowering prices to avoid cuts. By 2027, an estimated 35% of new drugs will undergo independent cost-effectiveness reviews by payers-up from 12% in 2022. Pressure from patients, insurers, and public opinion is growing. Change is slow, but it’s coming.
There’s no easy answer. But there’s a clear path: know your options, ask for help, and don’t let cost silence your voice.



Betty Kirby
February 14, 2026 AT 16:47 PM
Let’s be real-$500,000 for a drug that gives you six extra months of chemo-induced misery isn’t healthcare. It’s extortion dressed in white coats. I’ve seen families sell homes, max out credit cards, and still end up with nothing. The system isn’t broken. It was designed this way to profit off desperation.
And don’t get me started on ‘patient assistance programs.’ They’re not charity. They’re PR stunts. You need a PhD in bureaucracy just to qualify. Meanwhile, the same company that charges you $500k is lobbying Congress to block price caps. This isn’t capitalism. It’s feudalism with a pharmacy.
There’s no moral high ground here. Just greed. And we’re all paying for it-with our health, our savings, our dignity.