Cyclosporine Monitoring Calculator
Cyclosporine Safety Checker
Enter your recent test values to see if your cyclosporine levels and kidney function are within safe ranges.
Important: This calculator is for educational purposes only. Always follow your doctor's advice for your specific situation.
For most patients, cyclosporine levels should be measured 2 hours after taking the dose (C2) for the most accurate results.
Results
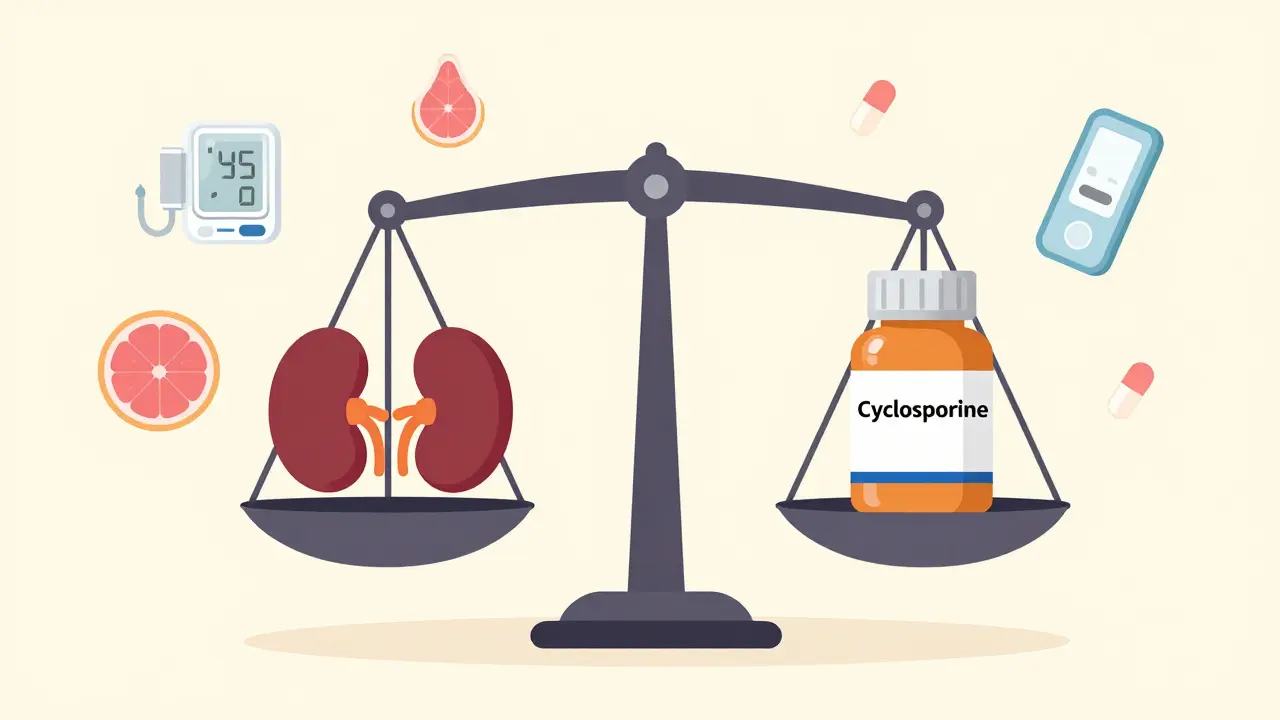
When you take cyclosporine after a kidney, heart, or liver transplant, it’s not just about preventing rejection. It’s about walking a tightrope. Too little, and your body attacks the new organ. Too much, and your kidneys start to fail. This isn’t theoretical-it happens in real time, every day, in transplant centers around the world. And the difference between safety and damage often comes down to one thing: cyclosporine levels and how closely you track your kidney function.
Why Cyclosporine Is a Double-Edged Sword
Cyclosporine, also known as ciclosporin, has saved hundreds of thousands of lives since the 1980s. It’s powerful. It stops your immune system from rejecting transplanted organs. But it doesn’t know the difference between a dangerous cell and a healthy one. And it doesn’t care. At high enough doses, it crushes the tiny blood vessels in your kidneys, raises your blood pressure, and slowly kills off kidney tissue. This isn’t a side effect-it’s the drug’s main danger. About 30% to 50% of long-term kidney transplant failures are tied directly to cyclosporine toxicity when monitoring isn’t tight.What makes this worse is that the line between working dose and toxic dose is razor-thin. One day your level might be 140 ng/mL-safe. The next, after a cold or a new antibiotic, it spikes to 210 ng/mL-dangerous. And you might not feel a thing until your creatinine climbs and your kidneys start slipping.
What You Need to Measure: More Than Just Cyclosporine
Monitoring cyclosporine isn’t just about checking the drug number. It’s a three-part system:- Cyclosporine blood levels - the drug concentration in your blood
- Kidney function markers - creatinine, BUN, magnesium, and blood pressure
- Drug interactions - what else you’re taking that could mess with absorption or metabolism
For kidney transplant patients, the target levels change over time. In the first week after surgery, doctors aim for 200-400 ng/mL. By six months, that drops to 100-150 ng/mL. After a year, 75-160 ng/mL is the sweet spot. Miss these targets, and you risk rejection or kidney damage. Heart and liver transplant patients have slightly different ranges, but the principle is the same: lower over time, but never too low.
But here’s the catch: if you’re only checking your trough level (the lowest point right before your next dose), you’re flying blind. Studies show that measuring your level two hours after taking the pill-called the C2 level-gives a much clearer picture of how much drug your body is actually absorbing. Centers using C2 monitoring cut nephrotoxicity by over 22% compared to those relying only on trough levels.
How Labs Measure Cyclosporine-And Why It Matters
Not all blood tests are created equal. There are three main ways labs measure cyclosporine:- LC-MS/MS (liquid chromatography-tandem mass spectrometry) - the new gold standard. Used in 92% of U.S. transplant centers as of 2021. It’s accurate, picks up only the real drug, not its metabolites, and can detect levels as low as 5 ng/mL.
- High-performance liquid chromatography (HPLC) - accurate but slow and expensive. Fewer labs use it now because LC-MS/MS is better and faster.
- Immunoassays - fast and cheap, but flawed. These tests can’t tell the difference between cyclosporine and its metabolites. That means your result might be 20-30% higher than reality. If you’re on an immunoassay and your level reads 180 ng/mL, you might actually be at 140 ng/mL-safe. Or worse, your level could be 160 ng/mL, but the test says 200 ng/mL, and your doctor cuts your dose too much, putting you at risk for rejection.
One study tracked 12,450 patients and found labs using immunoassays made 22% more dosing errors than those using LC-MS/MS. That’s not a small difference-it’s life or death.
What Your Kidney Numbers Should Look Like
Even if your cyclosporine level looks fine, your kidneys might already be under stress. That’s why you need to watch these markers:- Serum creatinine - should stay below 1.5 mg/dL. If it climbs above that, especially over several weeks, your kidneys are struggling.
- BUN-to-creatinine ratio - keep it under 20:1. A higher number suggests dehydration or reduced kidney blood flow.
- Magnesium - cyclosporine drains magnesium. Normal range is 1.7-2.2 mg/dL. Low magnesium means you’re losing electrolytes and your muscles or heart could be affected.
- Blood pressure - cyclosporine causes high blood pressure in up to 70% of users. Target is under 130/80 mmHg. Uncontrolled pressure speeds up kidney damage.
Uric acid levels are sometimes checked, but evidence is mixed. Don’t waste time on them unless your doctor sees a pattern.
Drugs That Can Blow Up Your Cyclosporine Levels
You can be taking the exact same dose for months, then add a single pill-and your cyclosporine skyrockets. Why? Because of liver enzymes.Cyclosporine is broken down by CYP3A4, a liver enzyme. Anything that blocks or speeds up this enzyme changes your drug levels dramatically:
- Increases cyclosporine by 30-50%: ketoconazole (antifungal), erythromycin, grapefruit juice, diltiazem, verapamil
- Decreases cyclosporine by 40-60%: rifampin (TB drug), phenytoin, St. John’s wort, carbamazepine
Even over-the-counter meds like certain antacids or antibiotics can interfere. That’s why you need to tell every doctor, pharmacist, or nurse you see-every time-that you’re on cyclosporine. No exceptions.
How Often Should You Get Tested?
Frequency depends on how long you’ve been on the drug:- First month post-transplant: twice a week
- Months 2-6: once a week
- Months 7-12: every other week
- After one year: monthly or as needed
But this isn’t a fixed schedule. If you get sick, start a new medication, or your creatinine jumps, you’ll need more frequent testing. Also, it takes 4-6 weeks for your body to reach steady state after a dose change. So don’t panic if your level looks off after a single adjustment. Wait, retest, then decide.
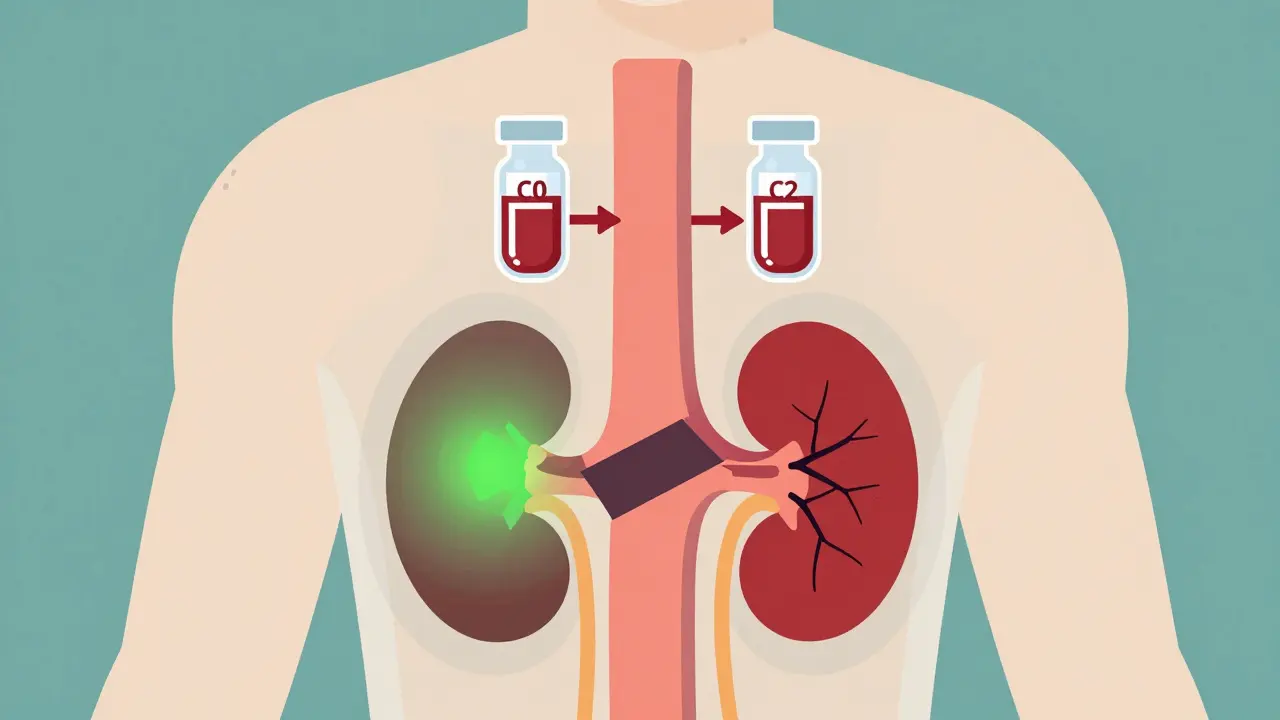
How Blood Samples Are Collected Matters-A Lot
You’d think drawing blood is simple. But if your blood goes into the wrong tube, your test result is wrong.Cyclosporine must be drawn into EDTA tubes (purple top). These preserve the drug in whole blood. If your lab uses serum separator tubes (red or gold top), you’ll get falsely elevated results-by 15-20%. That means your doctor might think you’re overdosing and cut your dose, risking rejection. Always confirm your lab uses EDTA tubes. If they don’t, ask for a referral to a center that does.

What’s New in Cyclosporine Monitoring
The field isn’t standing still. In 2023, guidelines started recommending genetic testing for CYP3A5. Some people are “extensive metabolizers”-their bodies clear cyclosporine fast. They need 30-40% higher doses to reach the same level as others. If you’ve had repeated rejection episodes despite “normal” levels, this could be why.Artificial intelligence is starting to help too. Trials are testing algorithms that predict your ideal dose based on your weight, age, liver function, genetics, and even your diet. Early results show 89.7% accuracy. That could mean fewer blood draws and better control.
By 2025, point-of-care devices are expected to hit the market. These handheld tools could measure your cyclosporine level from a finger prick in under 15 minutes. Imagine checking your level before your morning pill instead of waiting days for a lab result.
Can the Kidney Damage Be Reversed?
Yes-if caught early. Studies from the 1980s showed that when cyclosporine is reduced or stopped within three months of early kidney damage signs, function often improves. But if you wait too long, the damage becomes permanent. Arteries harden. Tubules scar. The kidney can’t repair itself.That’s why vigilance is everything. You can’t rely on symptoms. Nephrotoxicity doesn’t cause pain or fatigue until it’s advanced. You need numbers. You need consistency. You need to treat this like a daily job-not an occasional check-up.
What If You Can’t Tolerate Cyclosporine?
Some people just can’t handle it. Their kidneys keep failing despite careful monitoring. That’s when doctors switch to tacrolimus, sirolimus, or belatacept. Tacrolimus is more potent and has less nephrotoxicity at equivalent doses-but it still requires monitoring. Sirolimus is easier on the kidneys but can cause other issues like high cholesterol or mouth sores. There’s no perfect drug. But there is a better fit for every patient.If your creatinine keeps climbing and your doctor keeps raising your dose, ask: Is this still working? Or are we just trying to hold off the inevitable? Sometimes, switching drugs is the safest move.
How often should cyclosporine levels be checked after a kidney transplant?
In the first month after transplant, levels are checked twice a week. From months 2 to 6, weekly checks are standard. After six months, testing usually drops to every other week, and by year one, monthly checks are typical. But if your kidney function changes, you start a new medication, or you get sick, your doctor will increase the frequency.
Can grapefruit juice affect cyclosporine levels?
Yes. Grapefruit juice blocks the liver enzyme CYP3A4, which breaks down cyclosporine. This causes drug levels to rise by 30-50%, increasing the risk of kidney damage. Even one glass can have an effect that lasts over 24 hours. If you’re on cyclosporine, avoid grapefruit, pomelo, and Seville oranges entirely.
What’s the difference between C0 and C2 cyclosporine monitoring?
C0 is the trough level-measured right before your next dose. C2 is the level two hours after you take your pill. C2 correlates better with how much drug your body actually absorbs over time. Studies show C2 monitoring reduces nephrotoxicity by over 22% compared to C0 alone, and lowers rejection rates slightly. Many transplant centers now use C2 as their standard.
Why does my lab use a different test than my friend’s?
Not all labs use the same method. Some still use immunoassays because they’re cheaper and faster, but they can overestimate cyclosporine levels by 10-30%. Others use LC-MS/MS, which is more accurate but costlier. If your levels seem inconsistent or your doctor keeps adjusting your dose without clear reason, ask which method your lab uses and whether switching to LC-MS/MS might help.
Is cyclosporine nephrotoxicity always permanent?
No. If caught early-within the first few months of rising creatinine or high blood pressure-reducing the dose can lead to partial or full recovery of kidney function. But if high levels continue for over six months, the damage becomes structural and irreversible. Early detection through regular monitoring is the only way to prevent long-term harm.
Can I stop taking cyclosporine if my kidney function improves?
Never stop or change your dose without your transplant team’s approval. Even if your kidney numbers look good, stopping cyclosporine suddenly can trigger acute rejection, which can destroy your transplant within days. If your doctor considers reducing or switching your medication, it will be a slow, monitored process over weeks or months.
Managing cyclosporine isn’t about perfection. It’s about awareness. It’s about knowing your numbers, asking questions, and speaking up when something doesn’t feel right. Your transplant didn’t just give you a new organ-it gave you a responsibility. And that responsibility starts with understanding how this drug works, how it harms, and how to keep it in check.