Swallowing seems simple until it doesn’t work anymore. You eat a bite of food, and it just… sticks. No matter how much you drink, it won’t go down. That’s not just a bad day-it could be an esophageal motility disorder. These aren’t rare quirks of digestion. They’re real, measurable problems with how the esophagus moves food, and they’re often missed for years because they mimic acid reflux.
What Exactly Is Going On in Your Esophagus?
Your esophagus isn’t just a passive tube. It’s a muscular pipeline that contracts in a precise wave-like a peristaltic squeeze-to push food into your stomach. When those contractions get messy, too weak, or don’t relax properly, food gets stuck. That’s dysphagia: the feeling that something’s lodged in your throat or chest, even when there’s nothing there. This isn’t about heartburn. It’s about muscle failure. The most common cause? Achalasia. In this condition, the lower esophageal sphincter (LES)-the muscle that acts like a gate between your esophagus and stomach-won’t open. At the same time, the main body of the esophagus loses its ability to squeeze. Food piles up. People with achalasia often report progressive trouble swallowing solids, then liquids. Many lose weight. Some regurgitate undigested food hours after eating. It’s not laziness or anxiety. It’s a neurological-muscular breakdown. Other disorders include diffuse esophageal spasm, where random, uncoordinated contractions cause chest pain that feels like a heart attack. Then there’s nutcracker esophagus-contractions are strong but normal in timing, hitting pressures over 180 mmHg. And jackhammer esophagus, the most extreme form, with contractions so powerful they exceed 5,000 mmHg•s•cm. These aren’t just medical terms-they’re real, painful, life-limiting conditions.Why Manometry Is the Gold Standard
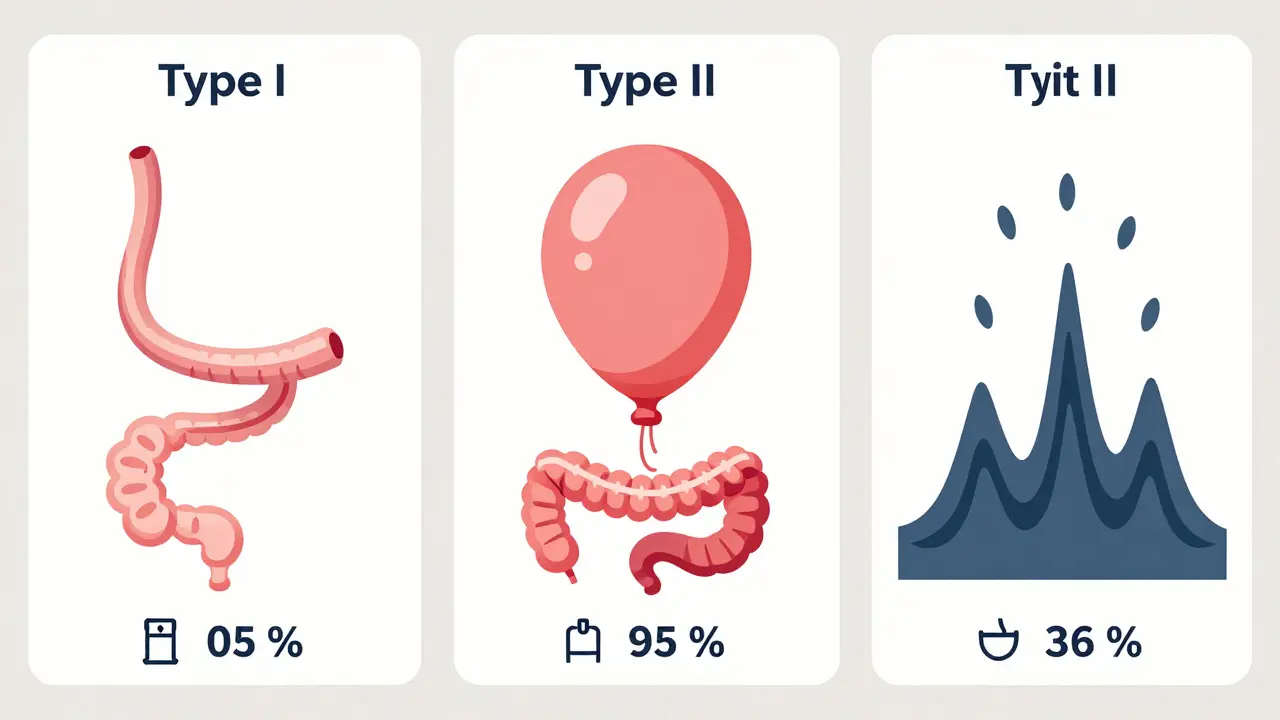
If you’ve had an endoscopy and they said, “Your esophagus looks fine,” but you still can’t swallow, you need manometry. Not just any manometry-high-resolution manometry (HRM). Traditional tests like barium swallows show you where food gets stuck, but not why. HRM uses a thin tube with 36 pressure sensors spaced 1 cm apart. As you swallow water, it maps every squeeze and relaxation in real time. The result? A color-coded pressure map that looks like a weather radar for your esophagus. This technology led to the Chicago Classification, first published in 2008 and updated in 2023 (v4.0). It’s the global standard for diagnosing these disorders. Before HRM, doctors disagreed on what they were seeing. Now, with clear criteria, diagnosis accuracy has jumped from moderate to excellent agreement-kappa values rose from 0.45 to 0.85. HRM doesn’t just spot achalasia. It breaks it into three types:- Type I (20%): No contractions at all-just a flaccid tube.
- Type II (70%): Pan-esophageal pressurization-your whole esophagus squeezes as one big balloon.
- Type III (10%): Spastic contractions-chaotic, forceful waves that don’t move food forward.
What About Other Tests?
Endoscopy is still the first step-just to rule out tumors, strictures, or Barrett’s esophagus. But if your esophagus looks normal and you still can’t swallow, HRM is the next and most important test. Barium swallow? It catches about 78% of achalasia cases. HRM catches 96%. That’s a huge difference. And while an MRI or CT scan might show anatomy, they can’t measure muscle function. There are newer tools too. EndoFLIP measures how stretchy your esophagus is, especially useful for identifying esophagogastric junction outflow obstruction (EGJOO)-a condition that mimics achalasia but has different treatment paths. And wireless manometry capsules, like the SmartPill, let you swallow a pill that records pressure for 24-48 hours as you go about your day. It’s less invasive, though not as detailed as HRM.
Why So Many People Are Misdiagnosed
Doctors see chest pain. They see regurgitation. They think GERD. So they prescribe proton pump inhibitors (PPIs). For years. That’s the trap. PPIs reduce acid. They don’t fix muscle dysfunction. A 2024 review in the Merck Manual found that many patients with motility disorders are treated as if they have reflux for 5-8 years before getting the right diagnosis. One patient posted online: “I took PPIs for eight years. My throat felt like sandpaper. Then manometry showed jackhammer esophagus. That’s when everything changed.” A survey of 1,247 patients found 68% waited 2-5 years for a correct diagnosis. Forty-two percent saw three or more doctors. Why? Because HRM isn’t available everywhere. It requires expensive equipment ($50,000-$75,000), specialized training, and time. Most community hospitals don’t have it. Only 35% of community hospitals in the U.S. offer HRM. In low-income countries, it’s under 10%.Treatment: From Surgery to New Tech
Once you have the diagnosis, treatment is targeted. For achalasia, the two main options are:- Laparoscopic Heller myotomy (LHM): Surgeons cut the LES muscle through small incisions. Success rate? 85-90% at five years. But about 29% develop reflux.
- Peroral endoscopic myotomy (POEM): A scope goes down your throat. A tunnel is made in the esophagus wall, and the muscle is cut from inside. It’s equally effective-but reflux rates are higher: 44% at two years.
What Patients Really Say
Real stories tell the real story. “I couldn’t eat bread or meat for seven years. After POEM? I had a burger. I cried.” - Reddit, March 2023 “I went to the ER three times thinking I was having a heart attack. Turns out, it was esophageal spasm.” - HealthUnlocked, January 2024 But not all experiences are positive. One patient said: “They told me it was anxiety. I was on antidepressants for a year before someone ordered manometry.” Patient satisfaction with HRM jumps from 45% to 78% when they’re properly prepared. That means explaining what the tube feels like, what swallowing water during the test will be like, and why it’s necessary. Most people tolerate it better than they expect.The Big Picture
Esophageal motility disorders are underdiagnosed, misunderstood, and often mismanaged. But they’re not mysterious. We have the tools. We have the science. We have the classification systems. The problem isn’t lack of knowledge-it’s access. HRM isn’t in every clinic. Training is limited. Many doctors still think “dysphagia = GERD.” If you’ve been told you have acid reflux but your meds don’t help-if you’re losing weight, regurgitating food, or getting chest pain that doesn’t respond to nitroglycerin-it’s time to ask for manometry. Not just any test. High-resolution manometry. The kind that follows the Chicago Classification v4.0. This isn’t about being “weird.” It’s about muscle function. And when you fix that, eating becomes normal again.15 Comments
Thomas Anderson
December 17, 2025 AT 02:09 AM
if you’ve been on PPIs for years and still can’t swallow bread, ask for HRM. it’s not fancy, it’s just the right test. no fluff, just numbers.
Dwayne hiers
December 18, 2025 AT 13:36 PM
the chicago classification v4.0 is a game-changer. type ii achalasia with pan-esophageal pressurization? that’s the classic pattern HRM catches. before this, we were guessing. now we’re mapping. the kappa jump from 0.45 to 0.85? that’s diagnostic clarity.
Jonny Moran
December 19, 2025 AT 12:24 PM
i’ve seen patients cry after POEM because they ate a burger for the first time in a decade. this isn’t just medicine-it’s restoring dignity. if you’re being told it’s anxiety, keep pushing. your body isn’t broken, it’s just misunderstood.
Sarthak Jain
December 20, 2025 AT 15:04 PM
in india, most docs still think dysphagia = acid. i had to travel 500km to find a center with hrmm. took 3 years. my mom cried when the report came back-type ii, not GERD. finally, a name for the pain.
Sinéad Griffin
December 21, 2025 AT 23:32 PM
PPIs are a scam. Big Pharma doesn’t want you to know your esophagus can fail without acid. HRM is expensive? good. keeps the riffraff out. if you’re not getting it, you’re not worth the time.
Natalie Koeber
December 22, 2025 AT 20:58 PM
you know who controls HRM machines? The same people who own the FDA. They buried the truth: 90% of these cases are caused by 5G radiation disrupting vagal nerve signaling. But you won’t hear that from your ‘gastroenterologist’ because they’re paid by the device manufacturers.
Rulich Pretorius
December 22, 2025 AT 23:53 PM
I’ve spent 20 years in clinical neurogastroenterology. The real tragedy isn’t the misdiagnosis-it’s the delay in access. HRM isn’t a luxury. It’s a basic diagnostic tool, like a stethoscope. If your hospital doesn’t have it, they’re not practicing medicine-they’re guessing.
Tim Bartik
December 24, 2025 AT 23:24 PM
POEM sounds like sci-fi. cutting muscle from INSIDE your throat with a scope? i’d rather swallow a live eel. but hey, if it lets me eat steak again, sign me up. my wife says i’ve become a different person since the surgery.
Edward Stevens
December 26, 2025 AT 20:45 PM
so let me get this straight. you’re telling me that for 8 years, people were getting antidepressants for a muscle disorder? and now we’re celebrating a 96% detection rate? wow. we really are geniuses.
Alexis Wright
December 28, 2025 AT 12:13 PM
The truth is, this entire field is a controlled narrative. HRM doesn’t measure motility-it measures compliance with a corporate protocol. The Chicago Classification? It’s a marketing tool. The real problem? The vagus nerve is being chemically silenced by glyphosate in our food supply. But don’t worry, your GI doc has a pamphlet.
Daniel Wevik
December 30, 2025 AT 11:54 AM
if you're reading this and you’ve been told 'it's just anxiety'-you’re not alone. but you’re not broken. this isn’t in your head. it’s in your muscles. HRM isn’t scary-it’s your key to freedom. ask for it. insist on it. your esophagus deserves to work.
Rich Robertson
January 1, 2026 AT 00:42 AM
i’m from rural pennsylvania. we don’t have HRM here. my sister drove 4 hours for hers. she got type iii. they did a myotomy. now she eats pizza on Sundays. that’s not medicine. that’s a miracle.
Wade Mercer
January 1, 2026 AT 09:06 AM
people who don’t get tested are just lazy. if you can’t swallow, you should’ve known better. this isn’t a mystery-it’s negligence. stop blaming the system. take responsibility.
Daniel Thompson
January 3, 2026 AT 04:05 AM
I appreciate the clinical rigor here, but I must emphasize the structural inequities. The $75,000 price tag on HRM equipment is not a technical limitation-it is a moral failure. Access to diagnostic precision should not be a function of ZIP code or insurance tier.





jeremy carroll
December 15, 2025 AT 12:59 PM
manometry? i thought they just gave you a barium milkshake and called it a day. turns out my throat issues were never heartburn, just my esophagus throwing a tantrum.