If your medication isn’t doing what it’s supposed to, you’re not alone. Around half of all people don’t take their meds as prescribed, and a big reason? They don’t feel like it’s helping. But here’s the thing: your doctor can’t fix what they don’t know. If you’re stuck with a pill that’s not working-or making things worse-you need to speak up. And there’s a smart, clear way to do it.
Start with the facts, not frustration
Don’t just say, "This isn’t working." That’s vague. Your doctor hears that a lot. Instead, get specific. Write down when you take the medicine, what symptoms you still have, and how bad they are. Did your pain go from an 8 to a 6? Still too high. Did you feel dizzy every afternoon after your pill? That’s a red flag. A 2022 study from University Health found that patients who brought detailed symptom logs were 68% more likely to get a real response. Bring a notebook. Use your phone. Just don’t rely on memory.
Also, bring your actual medicine bottles. Not a list. Not a photo. The real bottles. Why? Because pills look similar, and mistakes happen. One woman brought her meds to her appointment and realized her doctor had prescribed two drugs that interacted badly. That mix-up was caught because she showed the labels. University Health found that bringing bottles cuts medication errors by 22%.
Ask the right questions
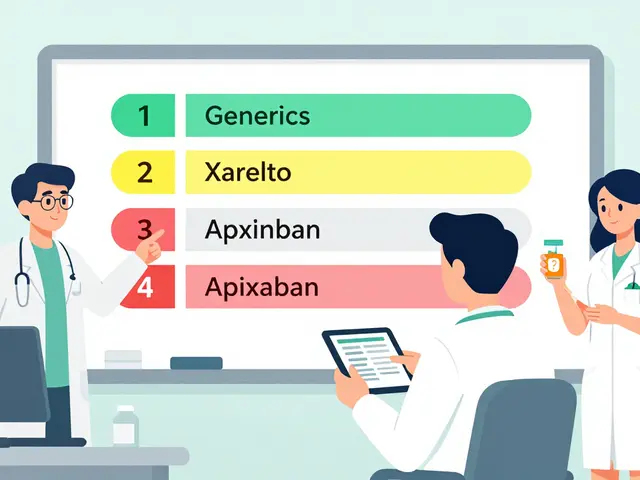
Here are the questions that actually move the needle, based on advice from the Deprescribing Network, MedlinePlus, and Harvard Health:
- "Why am I taking this?" Sometimes, a pill gets prescribed and just… stays. No one checks if it’s still needed.
- "What are the alternatives?" This isn’t asking for a list. It’s inviting a conversation.
- "What are the pros and cons of each option?" Some meds work better for certain symptoms. If you care more about daytime energy than nighttime sleep, say so.
- "Can I stop or reduce this?" Especially if you’re on multiple drugs, one might be unnecessary.
- "Could this affect my memory or balance?" Especially if you’re over 65. The American Geriatrics Society lists 34 meds that raise fall risk.
- "Is there a generic or cheaper version?" Sixty-two percent of people find lower-cost options when they ask.
Dr. Barbara Farrell, who helped start the Deprescribing Network, says patients who ask these kinds of questions are over three times more likely to have unneeded meds safely stopped. That’s not luck. That’s strategy.
Don’t wait for the next appointment
Too many people wait weeks to mention a problem. A 2022 JAMA Network Open study showed that 32% of patients held off until their next scheduled visit-even when the side effects were dangerous. That’s 30 extra days of feeling awful, or worse.
If something feels off, call the office. Ask for a nurse or pharmacist. Use your patient portal. Many clinics now let you send a note directly to your doctor’s inbox. Epic Systems rolled out a tool called MyMedList in late 2023 that lets you log concerns ahead of time. Your doctor sees it before the appointment. That means less time explaining, more time deciding.
Know your options beyond pills
When people say "alternative," they often mean another drug. But sometimes, the best alternative isn’t a pill at all.
- For sleep issues: Cognitive behavioral therapy for insomnia (CBT-I) works as well as sleeping pills-without the grogginess or fall risk.
- For type 2 diabetes: A 2022 study in Diabetes Care found that diet, exercise, and weight loss matched metformin’s effect on blood sugar in nearly 7 out of 10 people.
- For acid reflux: Cutting out spicy food, eating earlier, and losing weight helped 55% of people stop needing proton-pump inhibitors.
- For anxiety: Therapy, breathing exercises, and regular movement can be just as effective as SSRIs for mild-to-moderate cases, according to a Lancet Psychiatry meta-analysis.
- For back pain: The American College of Physicians now says exercise, acupuncture, and physical therapy should come before painkillers.
Ask: "Are there non-drug options I haven’t tried?" If your doctor says no, ask for a referral. Physical therapists, dietitians, and counselors are part of the team too.
Use your data
Pharmacogenomic testing-that’s DNA testing to see how your body processes drugs-is now available through many primary care clinics. It shows if you’re likely to have side effects or not respond to certain meds. Clinical data shows it helps pick the right drug for 57% of people. Ask: "Could genetic testing help us find a better fit?"
Also, check your clinical notes. If you use the same health system for everything, log in to your portal. See what your doctor wrote after your last visit. If they mentioned "poor response" or "side effects," use that as your opening line next time.

What if your doctor says no?
Forty-one percent of patients say they felt dismissed when asking for alternatives. That’s unacceptable. But here’s what you can do:
- Ask: "Can we get a second opinion?" Many insurers cover it.
- Request a referral to a specialist. A pharmacist, geriatrician, or pain specialist might see things differently.
- Ask for a written plan-even if it’s "monitor for 4 more weeks." That gives you a timeline and an out if things don’t improve.
- Get a copy of your prescription history. You own it. If a provider refuses to adjust, take it to someone else.
Medicare now pays doctors more to have longer medication reviews (up to $52 for 30 minutes). That means the system is starting to support these conversations. Use that.
Follow up
Don’t assume a new prescription fixes everything. Set a date-two weeks or a month-to check in. Did the new med help? Did it cause new side effects? Write it down. Bring it back. You’re not being difficult. You’re being smart.
People who understand their treatment and help make decisions stick with it 35% more often. That’s not just about compliance. It’s about control. You’re not just a patient. You’re the person living with this condition. Your input isn’t optional. It’s essential.
What if I’m scared to ask my doctor for alternatives?
It’s normal to feel nervous, but remember: your doctor’s job is to help you feel better. Most aren’t offended by questions-they’re relieved you spoke up. Start small: "I’ve been having trouble with this medication. Can we talk about other options?" That’s enough. You don’t need to be perfect. Just honest.
Can I switch medications on my own if this one isn’t working?
No. Stopping or switching meds without guidance can be dangerous. Some drugs need to be tapered. Others cause rebound effects. Even if you’re sure it’s not working, talk to your provider first. They can help you stop safely-or switch to something better.
How long should I wait before saying a medication isn’t working?
It depends. Some meds take weeks to build up. Others should work in days. Ask your doctor upfront: "How long should I wait before I know if this is working?" Write that down. If you hit that date and still feel the same, it’s time to talk. Don’t wait longer just because you’re unsure.
Is it worth asking about cost if the medication isn’t working?
Yes. Even if a drug isn’t working, cost can still be a factor. You might be paying for something that doesn’t help. Asking about generics or alternatives can open the door to something more effective-and cheaper. Sixty-two percent of patients who asked about cost found a better option.
What if my doctor says there are no alternatives?
That’s rare. There’s almost always another option-even if it’s a different dose, a non-drug therapy, or a referral. Ask: "Can you explain why you think there are no alternatives?" If the answer feels dismissive, request a second opinion. You have the right to understand your choices.