
Why Your Snoring Might Be Hurting Your Heart
If you snore loudly, wake up gasping for air, or feel exhausted even after a full night’s sleep, it’s not just annoying-it could be putting your heart at serious risk. Obstructive sleep apnea (OSA) affects about 1 billion adults worldwide, and most don’t even know they have it. But here’s the thing: OSA doesn’t just steal your rest. It silently damages your heart, raises your blood pressure, and makes dangerous heart rhythms far more likely.
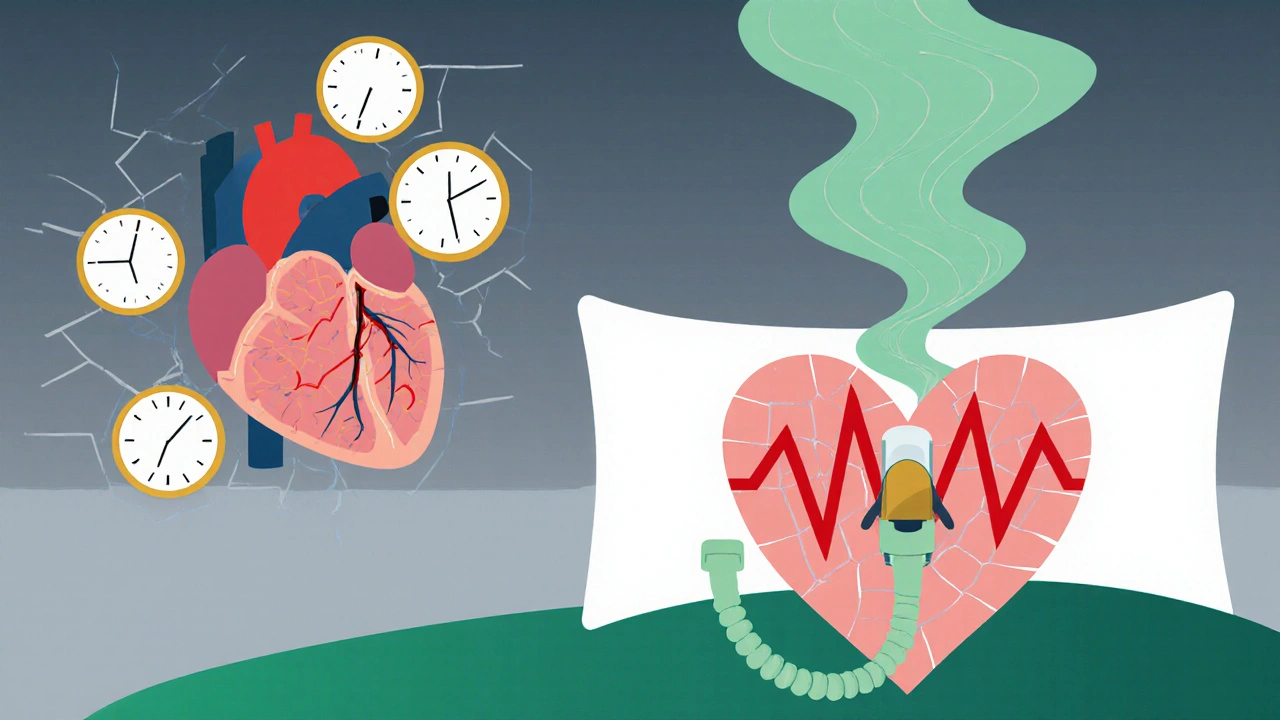
How Sleep Apnea Screws With Your Blood Pressure
Every time your airway collapses during sleep, your body panics. Oxygen drops. Your brain jolts you awake-just enough to breathe, but not enough for real rest. This happens dozens, sometimes hundreds, of times a night. Each time, your sympathetic nervous system fires like a alarm bell: “We’re suffocating!”
The result? Blood pressure spikes by 20 to 40 mmHg during each apnea. That’s like running a sprint every few minutes all night long. Over time, this pattern doesn’t fade when you wake up. It sticks around. Studies show people with untreated OSA are far more likely to have persistent high blood pressure-even if they’re young, thin, or otherwise healthy.
And it’s not just about the numbers. That constant pressure strain leads to thickened heart walls, stiffened arteries, and reduced blood flow to the heart muscle. About 35-45% of people with OSA already show signs of left ventricular diastolic dysfunction, meaning their heart can’t relax properly between beats. That’s the early warning sign of heart failure.
Why Your Heart Starts Skipping Beats
Arrhythmias-irregular heartbeats-are one of the most dangerous consequences of untreated sleep apnea. The same oxygen drops and nerve surges that spike your blood pressure also mess with your heart’s electrical system. Vagal tone drops. Sympathetic activity explodes. That imbalance creates the perfect storm for atrial fibrillation (AFib), the most common and dangerous type of arrhythmia.
People with severe OSA (30+ breathing pauses per hour) are three to five times more likely to develop AFib than those without sleep apnea. Even worse: OSA increases AFib risk by 140%, while high blood pressure only raises it by 50%. And here’s what most doctors still miss: this isn’t just an older person’s problem. New research from UT Southwestern shows OSA is increasing AFib rates in adults under 40, too.
It gets worse. Even after treating AFib with medication or ablation, patients with untreated OSA are far more likely to have it come back. One study found that consistent CPAP use cuts AFib recurrence by 42% after a year. That’s not a small boost-it’s life-changing.
OSA Is Worse Than You Think-And Easier to Fix
Many people assume obesity is the real culprit behind heart problems in sleep apnea patients. But research controls for weight, age, diabetes, and cholesterol-and OSA still stands out as an independent risk factor. It’s not just a side effect. It’s a direct cause.
Compare it to smoking: you don’t need to be overweight to get lung cancer from cigarettes. Similarly, you don’t need to be obese to get heart damage from OSA. Even mild cases (5-14 events per hour) raise stroke risk by 60% and coronary artery disease risk by 30%. And here’s the kicker: 45-65% of people with high blood pressure, AFib, or heart failure have undiagnosed sleep apnea.
That’s why the American Heart Association now says: if you have any of those conditions, you should be screened for OSA. Period. Yet only 20-25% of at-risk patients actually get tested.
CPAP Works-If You Use It
The gold standard treatment? Continuous Positive Airway Pressure (CPAP). It’s not glamorous. You wear a mask. You hear a quiet hum. But it works. Consistently.
On average, CPAP lowers systolic blood pressure by 5-10 mmHg. That’s the same drop you’d get from a low-dose blood pressure pill. For people with resistant hypertension (blood pressure still above 140/90 despite three medications), CPAP can be the missing piece.
And for arrhythmias? The data is clear. Patients who use CPAP 4+ hours a night see a 42% drop in AFib recurrence. One user on Reddit shared his numbers: after three months of consistent use, his blood pressure dropped from 160/95 to 128/82. Another said his AFib episodes went from weekly to once every two months.
Yes, the mask can feel weird. Yes, some people quit in the first year. But those who stick with it-especially those who adjust the humidity, try different mask types, or use the ramp feature-report better sleep, more energy, and fewer heart symptoms within 30 days.
What to Do If You Suspect Sleep Apnea
You don’t need a sleep lab to start. Home sleep tests are accurate for most people and covered by Medicare and most private insurers if you have symptoms plus one of these conditions:
- High blood pressure
- Atrial fibrillation
- Stroke
- Heart failure
- Resistant hypertension
Signs you should get tested:
- Loud, chronic snoring
- Gasping or choking during sleep (ask your partner)
- Waking up with a dry mouth or headache
- Daytime fatigue even after 8 hours of sleep
- Difficulty concentrating or mood swings
If you’re over 40 and have any of these, or under 40 with high blood pressure or AFib-get tested. Don’t wait for a heart attack to wake you up.
The Bigger Picture
The global market for sleep apnea devices is expected to hit $14.7 billion by 2028-not because people want fancy gadgets, but because doctors finally understand the stakes. OSA isn’t just a sleep problem. It’s a cardiovascular emergency hiding in plain sight.
Every time you ignore snoring, you’re ignoring your heart’s warning signs. But every time you use CPAP, you’re giving your heart a second chance. The science is no longer in question. The question now is: will you act before it’s too late?
14 Comments
Matthew McCraney
November 21, 2025 AT 18:45 PM
CPAP? That’s a big pharma scam. They don’t want you sleeping naturally. The mask? It’s a surveillance device. They’re tracking your breathing patterns to sell you ads for blood pressure meds. And don’t even get me started on the hum-that’s not a machine, that’s a mind-control frequency. I’ve been using a copper hat and salt lamps. My snoring’s louder but my soul’s free.
serge jane
November 23, 2025 AT 12:55 PM
It’s funny how we treat sleep like a luxury instead of the foundational architecture of health. We’ll spend hours optimizing our coffee, our gym routine, our protein shakes-but the eight hours that literally rebuild our cells? We treat it like background noise. OSA isn’t just a disorder-it’s the body screaming that we’ve forgotten how to rest. And the heart? It’s the canary in the coal mine, beating louder because we’ve stopped listening to silence.
Nick Naylor
November 24, 2025 AT 08:17 AM
The data is irrefutable. OSA is a direct, independent, and statistically significant cardiovascular risk multiplier. The American Heart Association guidelines are not suggestions-they are clinical imperatives. Failure to screen patients with hypertension, AFib, or heart failure constitutes negligence. Insurance companies are still treating this as a ‘sleep issue’-it’s not. It’s a systemic failure of medical prioritization. And CPAP compliance? That’s not a lifestyle choice. It’s a survival protocol.
Brianna Groleau
November 26, 2025 AT 03:05 AM
I used to think my husband’s snoring was just… loud. Then one night I woke up and he was gasping, his face blue-ish, and I swear my heart stopped. We got him tested. He’s been on CPAP for six months now. He sleeps like a baby. I sleep like a human. And he actually remembers our anniversary. I cried when he said, ‘I didn’t realize how tired I was.’ It’s not about the machine. It’s about being present. For your partner. For yourself. For the life you’re still breathing.
Sarah Swiatek
November 27, 2025 AT 13:49 PM
Oh wow, so the thing that’s been ruining my marriage for five years is also slowly killing my husband? Thanks for the update, science. I mean, I knew he was exhausted, but I thought it was just ‘midlife blahs.’ Turns out he’s got a silent death sentence and a $500 mask. Honestly? I’m glad we found out. Now I just need to convince him to stop using the ‘I’m not a robot’ excuse for not wearing it. Also, I’m getting tested. I snore too. Maybe I’m just a quiet heart-killer.
Dave Wooldridge
November 28, 2025 AT 00:37 AM
They’re hiding the truth. OSA isn’t natural-it’s caused by fluoride in the water. They put it in to make us sleepy so we don’t question the system. The CPAP machine? It’s just a cover-up. Real solution: sleep in a Faraday cage, drink raw apple cider vinegar, and sleep on a bed of Himalayan salt. I’ve been doing it for a year. My snoring’s gone. My dreams are lucid. The government hates me.
Rebecca Cosenza
November 28, 2025 AT 11:58 AM
I got tested after my dad had a stroke. Turns out I had mild OSA. Used CPAP for 3 weeks. My blood pressure dropped 15 points. I’m not a hero. I just didn’t want to die before my kids graduate. If you’re reading this and you snore… just do it. It’s not hard. Just wear the mask. Please.
swatantra kumar
November 29, 2025 AT 22:38 PM
Bro in India, same story. Snored like a chainsaw. Wife left me for 3 months. Got tested. CPAP. Now I sleep like a monk. Energy? 10x. Mood? Better than chai. My wife came back. Not because I changed. But because I stopped sounding like a dying buffalo. 😎❤️
Cinkoon Marketing
December 1, 2025 AT 00:16 AM
Honestly, I think people just need to sleep on their side. Or stop eating carbs after 6. Or maybe try a bamboo pillow. CPAP is overrated. I’ve got a friend who just uses a tennis ball sewn into his pajama back and he’s fine. No machine. No hassle. Just… better posture. Also, have you tried magnesium?
robert cardy solano
December 2, 2025 AT 23:02 PM
I used to think I was just a heavy sleeper. Turns out I was just unconscious for 20 seconds every 90 seconds. Woke up one day and realized I hadn’t felt fully awake in 12 years. CPAP was awkward at first. Now I forget I’m wearing it. Best decision I ever made. My dog stopped staring at me like I was dying. That’s saying something.
Pawan Jamwal
December 3, 2025 AT 05:37 AM
This is why India must develop its own CPAP tech. Why are we importing American masks? We have 1.4 billion people snoring. We need cheap, durable, solar-powered, desi CPAPs with chai-scented humidifiers. This isn’t just health-it’s national pride. We’ll make OSA history. 🇮🇳💪
Bill Camp
December 3, 2025 AT 14:10 PM
I’ve been ignoring this for years. My wife says I sound like a foghorn with a grudge. I thought it was just age. Now I’m 52, borderline hypertensive, and I just watched a video of myself choking in my sleep. I’m getting tested. No more ‘I’ll deal with it later.’ Later is when your heart says ‘nope.’
Lemmy Coco
December 4, 2025 AT 12:32 PM
i got cpap last year… kinda forgot to wear it for 3 months… then woke up one day and my head felt like a balloon… went back to it… 2 weeks later i could think again… like my brain had been on 20% battery for 10 years… still hate the mask tho… but i dont hate my heart anymore




rob lafata
November 20, 2025 AT 19:56 PM
So let me get this straight-you’re telling me my 3 a.m. snoring symphony is basically me doing interval training on my own heart? That’s not a bad night’s sleep, that’s a cardiac endurance test. And I thought my wife’s side-eye was the real punishment. Turns out she’s just a silent cardio coach. I’m getting tested tomorrow. No excuses.