Gut-Brain Axis: How Your Digestive System Shapes Your Mood, Sleep, and Medication Response
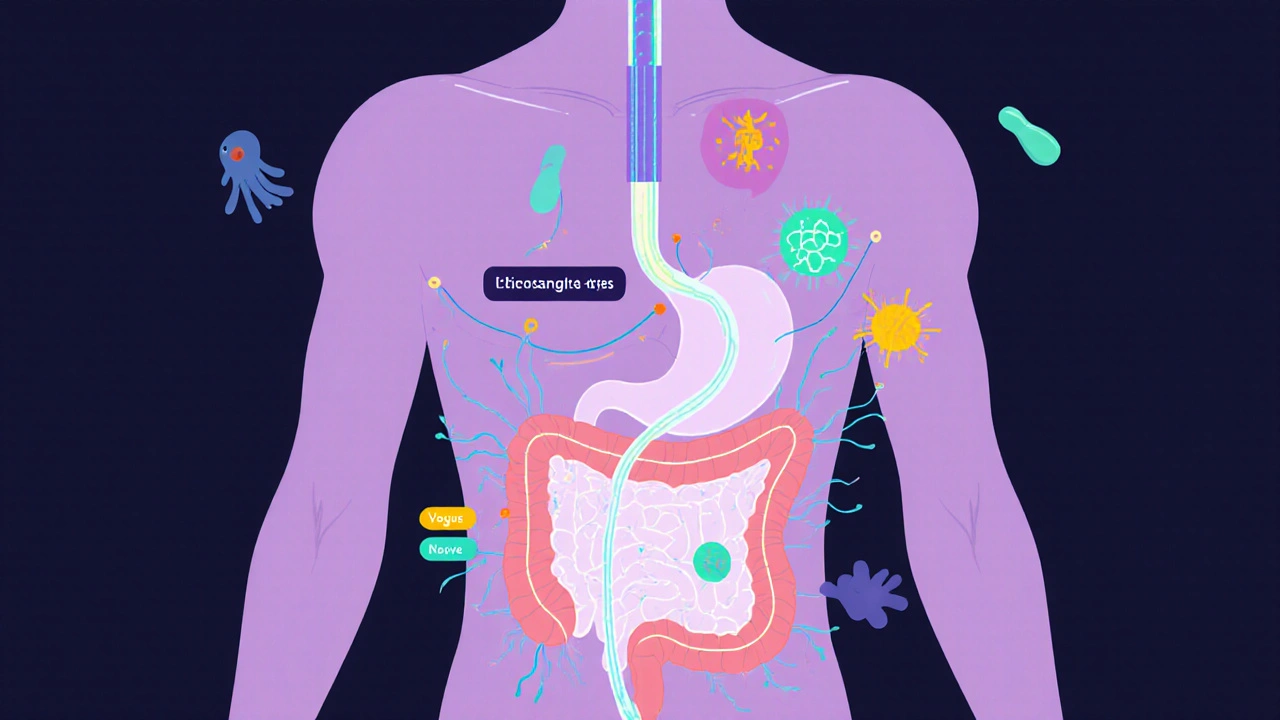
When you feel butterflies before a big meeting or get nauseous when stressed, you’re not imagining it—you’re experiencing the gut-brain axis, the two-way communication system between your digestive tract and your central nervous system. Also known as the enteric nervous system, it’s not just about digestion—it’s about how your gut talks to your brain, and how your brain changes what’s happening in your intestines.
This connection runs through the vagus nerve, the main nerve linking your brainstem to your abdomen, carrying signals in both directions. It’s why people with chronic gut issues like IBS often have higher rates of anxiety and depression. And it’s why some antidepressants cause stomach upset, while certain probiotics may help ease low mood. The microbiome, the trillions of bacteria living in your intestines produce over 90% of your body’s serotonin—a key neurotransmitter for mood and sleep. When these bacteria are out of balance, thanks to antibiotics, poor diet, or stress, they send signals that can alter your brain chemistry.
This isn’t just theory. Studies show that people taking medications like SSRIs, PPIs, or even antibiotics can see changes in their mental state because those drugs alter gut bacteria. For example, proton pump inhibitors—commonly used for heartburn—can reduce stomach acid enough to let harmful bacteria overgrow, which then triggers inflammation that travels to the brain. Meanwhile, antibiotics wipe out good bugs that help regulate sleep cycles, which may explain why some people struggle with insomnia after a course of pills. Even something as simple as eating a high-sugar meal can send a signal to your brain that makes you crave more, creating a loop that’s hard to break.
And it’s not just about mental health. The gut-brain axis affects how your body absorbs drugs, how you respond to pain, and even how well your immune system works. That’s why some people get side effects from medications others tolerate just fine—it’s not just about liver enzymes or kidney function. It’s about what’s happening in your gut. If you’ve ever wondered why your sleep doesn’t improve with melatonin, or why your anxiety spikes after eating certain foods, the answer might be in your microbiome.
What you’ll find in the posts below are real-world connections between gut health and the medications and conditions you’re likely dealing with. From how antibiotics trigger C. difficile infections that mess with your mood, to how sleep apnea and gut inflammation feed off each other, to why certain pain meds work better for some than others—these aren’t random topics. They’re all tied together by the same hidden system: your gut-brain axis. You’re not just reading about drugs. You’re reading about how your body really works.
Irritable Bowel Syndrome: Understanding the Gut-Brain Axis for Real Symptom Relief
Irritable Bowel Syndrome isn't just digestive trouble-it's a breakdown in gut-brain communication. Learn how stress, microbes, and nerve signals drive symptoms, and what actually works to restore balance and find lasting relief.
View More