Immune Response: How Your Body Fights Threats
When you hear the term Immune Response, the body's natural reaction to harmful invaders like viruses, bacteria, or abnormal cells. Also known as immune reaction, it kickstarts a cascade of defenses that keep you healthy. This reaction isn’t a single event; it’s a series of steps that involve detection, signaling, and elimination. Understanding those steps helps you see why certain medicines work and how lifestyle choices can boost your defenses.
The Immune System, a complex network of organs, cells, and proteins that patrol the body for danger is the platform that powers the immune response. Think of it as a security team: white‑blood cells patrol, the spleen stores reserves, and lymph nodes act as checkpoints. When a pathogen shows up, the system sends out alarm signals called cytokines, which rally the troops and start the fight.
Key Components of the Immune Response
One of the most visible weapons in the arsenal is the Antibody, a protein that specifically binds to foreign invaders and marks them for destruction. Antibodies are produced by B‑cells after they recognize a germ’s unique shape. The more you’re exposed (through infection or vaccination), the smarter your antibody library becomes, allowing quicker and stronger attacks on repeat offenders.
Vaccines, prepared substances that safely mimic pathogens to train the immune system exploit this learning process. By introducing a harmless piece of a virus or bacterium, vaccines teach the immune response to recognize the real threat without causing disease. The result is a faster, more efficient antibody production the next time the pathogen tries to invade.
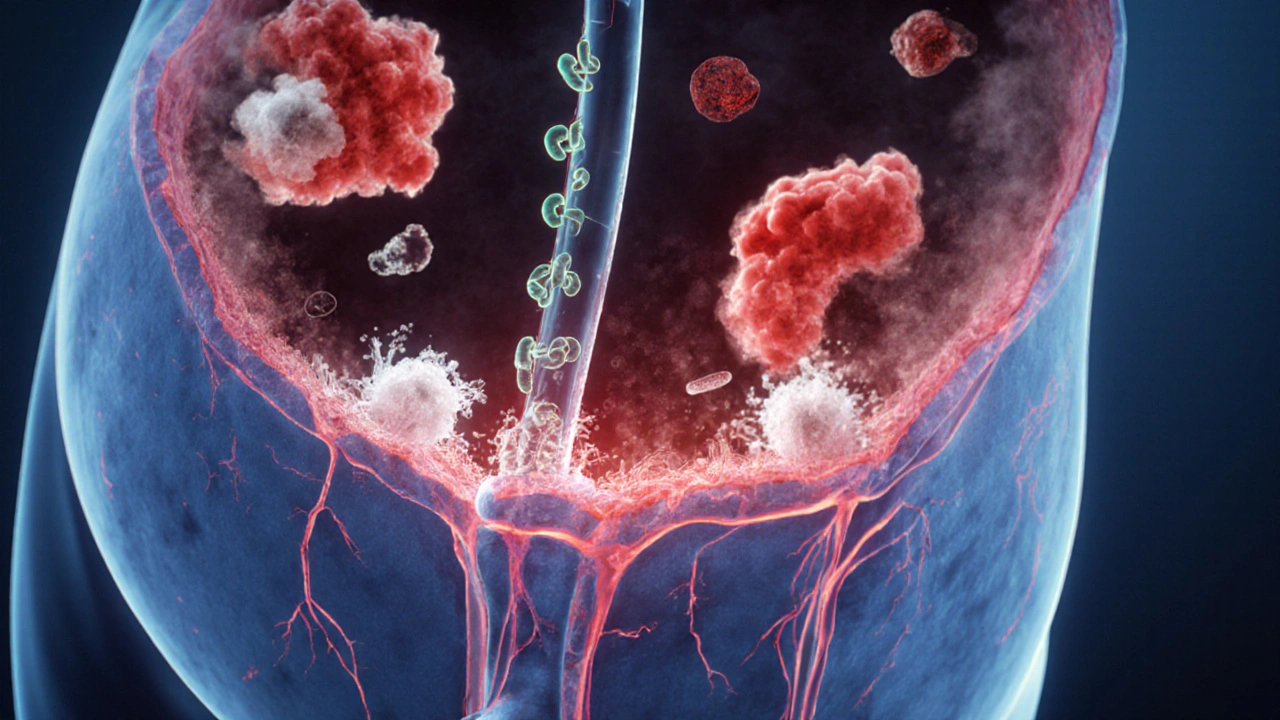
Immunotherapy, a treatment approach that harnesses or modifies the immune response to combat diseases like cancer takes the concept a step further. Instead of just supporting the natural response, it re‑programs immune cells to attack tumors, blocks signals that suppress immunity, or supplies synthetic antibodies that home in on cancer cells. It’s a clear example of how understanding the immune response can lead to breakthrough therapies.
The relationship among these entities forms a logical chain: the immune response encompasses antibody production; vaccines train the immune system; immunotherapy leverages that trained response to treat disease. Each link strengthens the next, creating a network where a single improvement—like a better vaccine—can boost overall health outcomes.
Lifestyle factors also shape the immune response. Adequate sleep, regular exercise, and balanced nutrition provide the raw materials immune cells need to function. For instance, vitamin C supports the production of white‑blood cells, while omega‑3 fatty acids modulate inflammation, preventing an over‑reactive response that can damage tissues.
Stress, on the other hand, can dampen the response. Chronic cortisol release lowers the activity of T‑cells and reduces antibody quality, making you more susceptible to infections. Simple stress‑management techniques—like deep breathing or short walks—can restore a healthier balance.
Age plays a role too. As we get older, the immune system’s ability to generate new antibodies declines, a phenomenon called immunosenescence. This explains why older adults benefit more from high‑dose flu vaccines and why immunotherapy doses often need adjusting for senior patients.
Genetics also leave a fingerprint on the immune response. Certain gene variants affect how receptors recognize pathogens, influencing everything from allergy severity to vaccine effectiveness. While you can’t change your DNA, knowing your genetic predispositions can guide personalized prevention strategies.
Environmental exposures—air quality, pollutants, and even gut microbiota—feed back into the immune response. A diverse gut microbiome educates immune cells, teaching them to tolerate harmless microbes while staying alert for true threats. Antibiotic overuse can disrupt this balance, leading to weaker defenses or autoimmune flare‑ups.
By grasping how the immune response interacts with antibodies, vaccines, immunotherapy, and lifestyle, you gain a roadmap for staying healthy and making informed medical choices. Below you’ll find a carefully curated set of articles that dive deeper into each of these facets, from comparing specific drugs to practical tips for boosting your own immunity.
UTI and Chronic Fatigue Syndrome: How Infections Trigger Fatigue
Explore how urinary tract infections can trigger chronic fatigue syndrome, the shared biological pathways, evidence, prevention tips, and steps to manage post‑UTI fatigue.
View More