Pharmacist Collaboration: How Teams Improve Medication Safety and Outcomes
When it comes to taking meds safely, pharmacist collaboration, the structured partnership between pharmacists and other healthcare providers to optimize medication use. Also known as interprofessional care, it’s not a nice-to-have—it’s the difference between a drug working as intended and causing a hospital visit. You might think your doctor handles everything, but pharmacists are the ones who catch the hidden dangers: that antibiotic clashing with your blood thinner, the sleep aid making your blood pressure spike, or the generic version with a filler that triggers a reaction. They don’t just count pills—they connect the dots.
Real pharmacist collaboration means a pharmacist is in the room—or on the call—with your doctor, nurse, and sometimes even you. It’s how patients on chemo avoid deadly interactions, how seniors on five different pills don’t end up in delirium, and how someone with a penicillin allergy gets flagged before the script is filled. This isn’t theory. Studies show when pharmacists actively review med lists and communicate with prescribers, hospital readmissions drop by up to 30%. That’s not magic. That’s someone checking if your OTC painkiller is safe with your kidney meds, or if your new antidepressant might mess with your heart rhythm. It’s also how REMS programs get enforced, how DRESS syndrome gets spotted early, and how expired meds or inactive ingredient clashes are caught before they hurt you.
Pharmacist collaboration doesn’t just happen in hospitals. It’s happening in community pharmacies where you pick up your prescriptions, in telehealth visits where a pharmacist reviews your full list, and in nursing homes where they adjust doses for aging bodies. It’s the reason you’re asked if you’re taking supplements, why your pharmacist calls when your new script looks risky, and why some meds come with special warnings only a trained eye would notice. This is the quiet work that keeps people out of the ER.
Below, you’ll find real cases where pharmacist collaboration made the difference—whether it was spotting a dangerous combo of antivirals and liver enzymes, catching an antifungal that wouldn’t absorb because of a proton pump inhibitor, or helping someone with shift work sleep disorder avoid meds that made their rhythm worse. These aren’t hypotheticals. These are stories of people who got the right care because someone took the time to look closer.

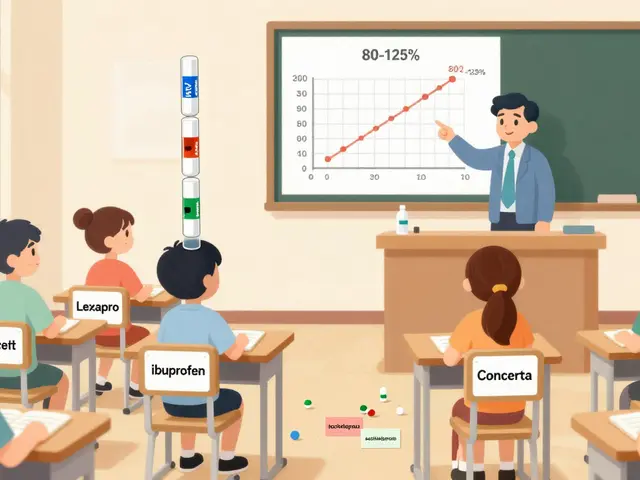
Team-Based Care: How Multidisciplinary Teams Improve Generic Prescribing Outcomes
Team-based care improves generic prescribing by combining doctors, pharmacists, and nurses to reduce errors, lower costs, and boost adherence. Learn how multidisciplinary teams are changing medication management for chronic conditions.
View More