Proton Pump Inhibitors: What They Are, How They Work, and What You Need to Know
When you hear proton pump inhibitors, a class of medications that block acid production in the stomach. Also known as PPIs, they’re among the most prescribed drugs in the world for heartburn, acid reflux, and ulcers. But they’re not harmless. While they work great short-term, taking them for years without a clear reason can lead to real problems—like nutrient deficiencies, bone loss, and even kidney issues. You might not realize it, but if you’ve been popping a pill every morning for more than a few months, you could be at risk.
Proton pump inhibitors work by targeting the tiny pumps in your stomach lining that produce acid. When these pumps are turned off, less acid flows into your stomach, which helps heal damage from reflux or ulcers. Common ones include omeprazole, esomeprazole, lansoprazole, and pantoprazole. You’ll find them over the counter and by prescription. But here’s the catch: many people stay on them way longer than they need to. A 2021 study in JAMA Internal Medicine found that nearly 70% of long-term PPI users had no documented reason for continuing them. That’s not because they’re ineffective—it’s because stopping them can cause rebound acid reflux, which feels like the original problem came back worse.
That’s where things get tricky. If you’ve been using PPIs for years, quitting cold turkey isn’t safe. Your stomach overcompensates by making even more acid than before. That’s why doctors often recommend tapering off slowly, switching to H2 blockers like famotidine, or using lifestyle changes—like eating smaller meals, avoiding late-night snacks, and cutting back on caffeine and alcohol. And if you’re on a PPI for heartburn but never got tested for H. pylori (a bacteria that causes ulcers), you might be treating a symptom instead of the cause.
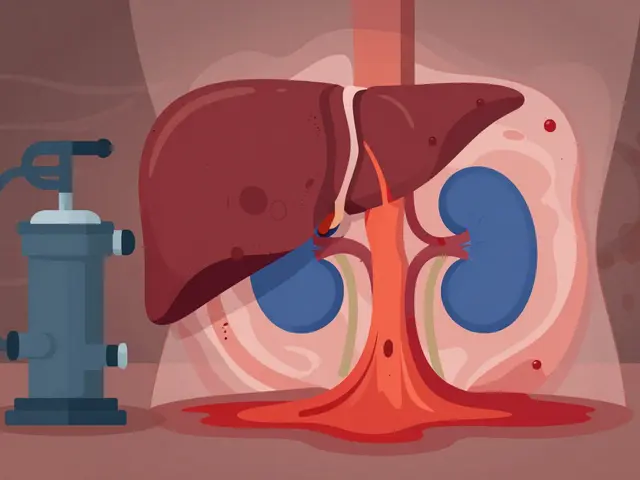
These drugs also affect how your body absorbs nutrients. Long-term use can lower levels of magnesium, calcium, and vitamin B12. That’s why people on PPIs for years sometimes end up with muscle cramps, fatigue, or even osteoporosis. And while they’re great for treating GERD, they’re not always the best first step. For mild cases, antacids or H2 blockers often work just as well—with fewer side effects.
What you’ll find in the posts below isn’t just a list of drug facts. It’s a collection of real-world stories and warnings from people who’ve been there: the woman who stopped PPIs and found her chronic bloating vanished, the man who developed kidney inflammation after five years on omeprazole, the doctor who explains why some patients need these drugs for life—and others don’t. You’ll also see how PPIs interact with other meds, what to do if you’re prescribed one without a clear diagnosis, and how to talk to your doctor about getting off them safely.
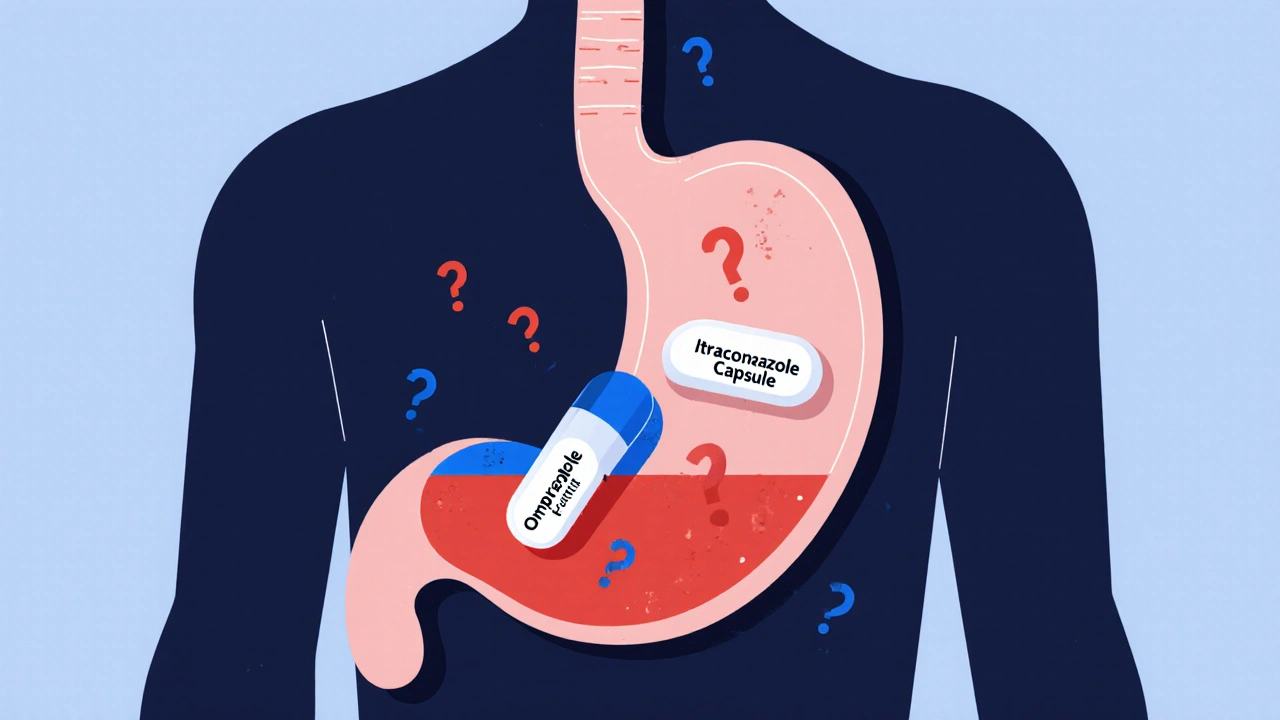
Proton Pump Inhibitors and Antifungals: How They Interfere with Absorption
Proton pump inhibitors can block the absorption of key antifungals like itraconazole, leading to treatment failure. Learn which drugs interact, how to fix it, and what new options are available.
View More