Step Counts: What They Really Mean for Your Health and Medications
When you hear step counts, the number of steps taken in a day, often tracked by wearables to measure physical activity. Also known as daily movement, it's not just about hitting 10,000—it's about how your body reacts to motion while on medication, recovering from illness, or managing long-term conditions. Many people think more steps automatically means better health, but that’s not always true. If you’re on blood pressure meds, diuretics, or antidepressants, your body might respond differently to movement than someone who isn’t. A sudden jump in steps can raise your heart rate too fast, make you dizzy from low sodium, or worsen fatigue from drugs like trazodone or amitriptyline.
Sedentary lifestyle, a pattern of little to no physical activity that increases risk for heart disease, diabetes, and muscle loss. Also known as inactivity, it’s not just about sitting too long—it’s about how it changes how your body absorbs and processes drugs. For example, if you’re on lamotrigine for mood control or proton pump inhibitors for acid reflux, being inactive can slow how your liver and kidneys clear those drugs. That means even normal doses might build up and cause side effects. On the flip side, if you suddenly start walking 8,000 steps a day after months of sitting, your kidneys might struggle to adjust, especially if you’re taking diuretics or NSAIDs. That’s when you risk dehydration, low potassium, or even kidney stress—something people don’t always connect to their step tracker.
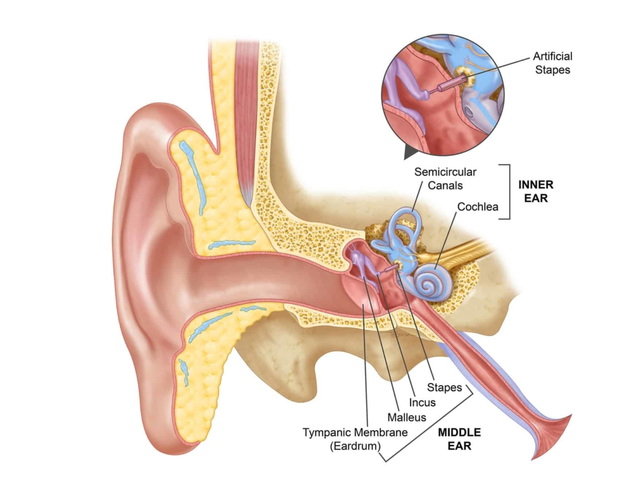
Step counts also matter when you’re dealing with chronic conditions like chronic kidney disease, a gradual loss of kidney function over time, often caused by diabetes or high blood pressure. Also known as CKD, it affects how your body handles movement and medication. If your eGFR is low, too much walking can strain your kidneys, especially if you’re dehydrated or on blood thinners. But too little movement? That speeds up muscle loss and makes blood pressure harder to control. It’s a tight balance. Same goes for people with fibromyalgia or diabetic neuropathy—gentle, consistent steps can ease pain, but pushing too hard can flare symptoms. And if you’re on opioids or anticholinergics, fatigue and dizziness from those drugs can make even 3,000 steps feel overwhelming.
What you’ll find in these articles isn’t just advice on how many steps to take. It’s about how your meds, your movement, and your body’s chemistry all talk to each other. You’ll see how fluoroquinolones can weaken tendons and make walking risky, how shift work messes with your natural rhythm and makes step goals harder to hit, and why expired meds or drug interactions can make you feel worse after a walk. This isn’t about fitness influencers or apps pushing you to break records. It’s about real people on real meds trying to move safely—without crashing their health.
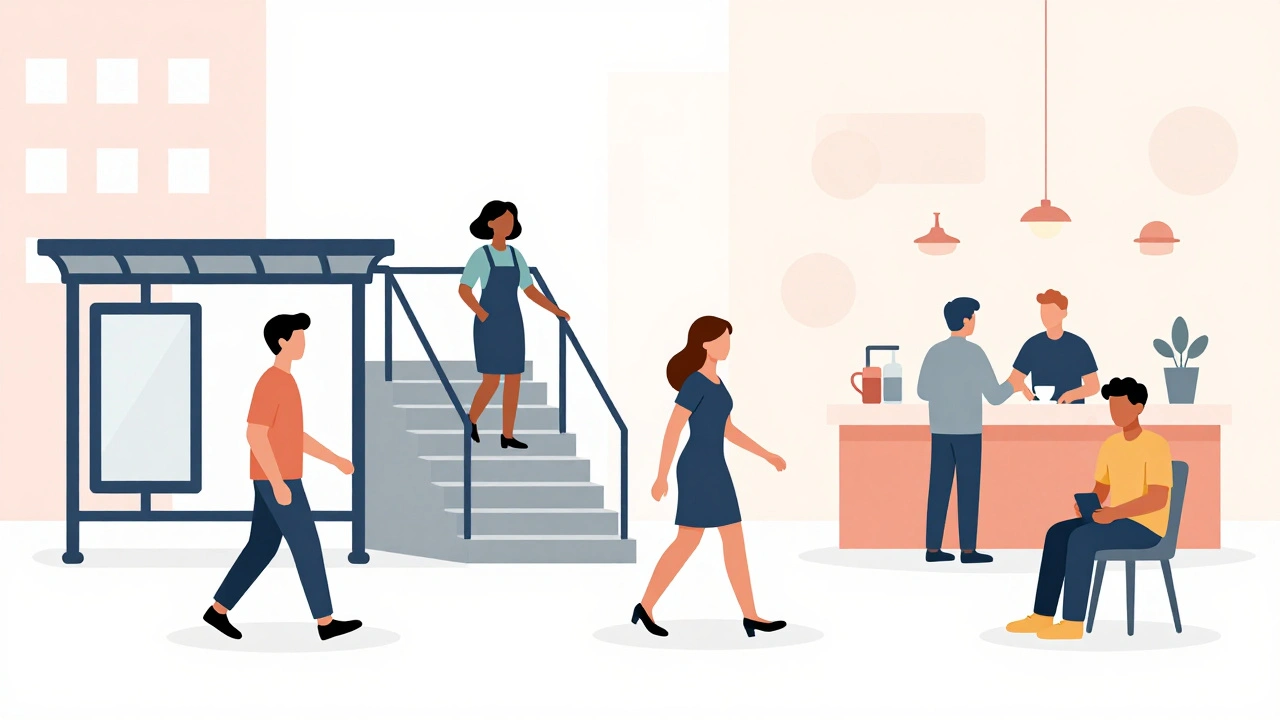
Step Counts and NEAT: How Daily Movement Burns Calories for Weight Management
Discover how daily movement like walking, standing, and climbing stairs-known as NEAT-burns calories without formal exercise. Learn how step counts truly impact weight management and why small moves add up over time.
View More