Tramadol Medication Interaction Checker
Check Your Medication Risk
This tool helps you understand if your current medications might interact with tramadol to cause serotonin syndrome. Tramadol can cause this dangerous condition even when taken alone or with other common medications.
Most people think of opioids as drugs that just block pain. But tramadol isn’t like morphine, oxycodone, or fentanyl. It’s different. And that difference can be deadly if you don’t know what you’re dealing with. Tramadol doesn’t just act on opioid receptors-it also messes with serotonin in your brain. That’s why it can cause serotonin syndrome, even when taken exactly as prescribed. This isn’t a rare side effect. It’s a well-documented, preventable emergency that happens more often than most doctors admit.
Why Tramadol Is Not Like Other Opioids
Traditional opioids like hydrocodone or codeine work one way: they bind to mu-opioid receptors in your brain and spinal cord. That’s it. Tramadol? It’s a double agent. About 6,000 times weaker than morphine at binding to opioid receptors, it makes up for it by blocking the reuptake of serotonin and norepinephrine. That’s the same mechanism used by antidepressants like SSRIs and SNRIs. So while morphine might make you sleepy or constipated, tramadol can send your serotonin levels soaring-especially if you’re already taking something that boosts serotonin.This dual action is why tramadol can cause serotonin syndrome without any other drugs involved. A 42-year-old woman in a 2011 case report took two 50 mg tablets of tramadol-nothing else-and ended up with high fever, muscle rigidity, and confusion. She didn’t overdose. She didn’t mix drugs. She just took what her doctor prescribed. And within hours, her body went into overdrive.
What Is Serotonin Syndrome? (And Why It’s Scary)
Serotonin syndrome isn’t just “feeling weird.” It’s a life-threatening condition where your nervous system gets flooded with too much serotonin. Symptoms can start within hours and escalate fast:- Shivering or muscle twitching (clonus)
- High fever (over 38°C or 100.4°F)
- Fast heartbeat, high blood pressure
- Sweating, dilated pupils
- Agitation, confusion, hallucinations
- Severe muscle stiffness or spasms
In extreme cases, body temperature can hit 41.2°C (106°F), leading to organ failure. A 35-year-old man in 2013 developed these symptoms after taking tramadol with fluoxetine. He spent three days in intensive care. He survived-but not everyone does.
The Hunter Criteria is the gold standard for diagnosis. You don’t need all the symptoms. Just one of these:
- Spontaneous clonus
- Inducible clonus + agitation or sweating
- Ocular clonus + agitation or sweating
- Tremor + hyperreflexia
- Hypertonia + fever + clonus
If you have even one of these after starting or increasing tramadol, stop it immediately and get help.
Who’s at Risk? (It’s Not Just Drug Mixes)
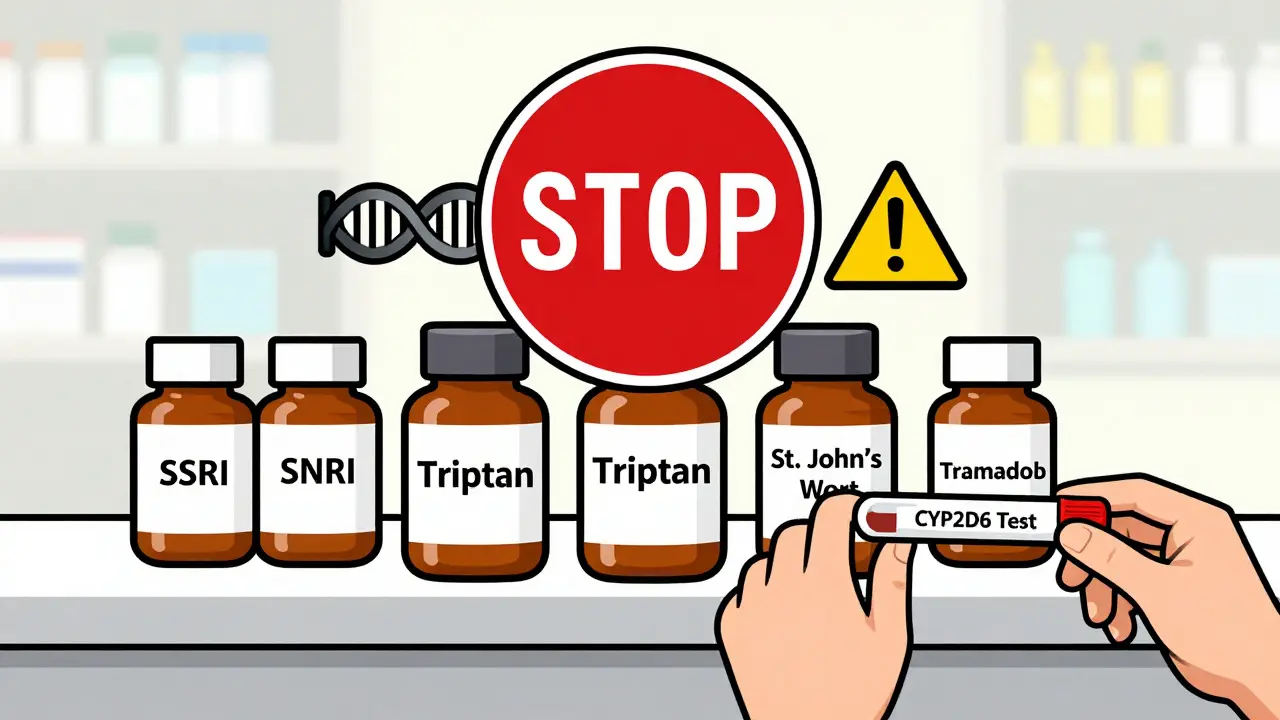
Many assume serotonin syndrome only happens when you combine tramadol with an SSRI like sertraline or fluoxetine. That’s true-but it’s not the whole story.Up to 7% of white people are “poor metabolizers” of tramadol because of a genetic variation in the CYP2D6 enzyme. This means their bodies can’t break down tramadol properly. The result? Higher levels of the active, serotonin-boosting form of the drug. These people can develop serotonin syndrome even on a normal dose-no other meds needed.
And it’s not just SSRIs. Other common drugs that raise serotonin risk when mixed with tramadol include:
- SNRIs (venlafaxine, duloxetine)
- MAOIs (phenelzine, selegiline)
- Triptans (sumatriptan for migraines)
- Linezolid (an antibiotic)
- St. John’s Wort (herbal supplement)
- Some cough syrups with dextromethorphan
A 2015 study of 187,000 Medicare patients found tramadol combined with an SSRI increased serotonin syndrome risk by 3.6 times. That’s not a small number. That’s a red flag.

Tramadol Alone Can Trigger It-And Doctors Often Miss It
A 2021 study in Pharmacotherapy found only 28% of tramadol-induced serotonin syndrome cases are correctly diagnosed. Why? Because symptoms look like other things:- Flu or infection (fever, sweating)
- Drug withdrawal (anxiety, tremors)
- Neuroleptic malignant syndrome (muscle rigidity)
One patient in a Reddit thread wrote: “I didn’t realize my 50 mg tramadol was interacting with my Lexapro until I ended up in the ER with a 104°F fever.” He wasn’t taking too much. He wasn’t mixing drugs recklessly. He was following his prescriptions. And still, his body reacted.
Even the FDA got involved. In 2011, they added a black box warning to tramadol for seizure risk at doses over 400 mg/day. But they didn’t stop there. In 2014, they reclassified it as a Schedule II controlled substance because of abuse potential and dangerous interactions. That didn’t stop prescriptions-it just made them harder to get.
What to Do If You’re Taking Tramadol
If you’re on tramadol right now, here’s what you need to do:- Check your other meds. Go through every pill, patch, or supplement you take. Look for SSRIs, SNRIs, triptans, or St. John’s Wort.
- Know your symptoms. If you feel unusually anxious, sweaty, shaky, or your muscles feel tight, don’t wait. Call your doctor or go to urgent care.
- Don’t stop cold turkey. If you need to stop tramadol, do it slowly under medical supervision. Sudden withdrawal can cause seizures or severe anxiety.
- Ask about CYP2D6 testing. If you’re Caucasian and have had unexplained side effects from tramadol, ask if genetic testing is an option. It’s not routine-but it should be.
If you’re prescribed tramadol for neuropathic pain and you have depression, anxiety, or bipolar disorder, talk to your doctor about alternatives. Tapentadol, for example, works on opioid receptors and norepinephrine-but has almost no effect on serotonin. A 2023 NIH study found tapentadol caused 63% fewer cases of serotonin syndrome than tramadol.
What’s Being Done About It?
The European Medicines Agency called tramadol’s risk-benefit profile “unacceptable” for patients with psychiatric conditions-and they’re considering restrictions by 2025. In the U.S., the CDC’s 2022 opioid guidelines specifically warn that tramadol has “unique serotonergic risks not shared by other opioids.”Researchers are now testing new versions of tramadol that keep the pain relief but remove the serotonin effect. One compound, called M1-tramadol, is in Phase II trials. It’s too early to say if it’ll work-but the goal is clear: make pain relief safer.
Meanwhile, hospitals are starting to use the Hunter Criteria more consistently in ERs. And some clinics now screen for CYP2D6 status before prescribing tramadol. But most still don’t. That’s on you to ask for.
Bottom Line: Tramadol Isn’t Safe Just Because It’s Prescribed
Just because your doctor wrote a prescription doesn’t mean it’s risk-free. Tramadol is not a generic opioid. It’s a serotonin-modifying drug with a hidden danger that even many clinicians overlook. If you’re taking it-and especially if you’re on any antidepressant-know the signs. Don’t assume you’re safe because you’re not overdosing. Serotonin syndrome doesn’t care about your dose. It cares about your chemistry.If you’ve ever felt off after starting tramadol-unexplained sweating, tremors, confusion-don’t brush it off. That could be your body screaming for help. Talk to your doctor. Get tested. Switch if needed. Your life might depend on it.
Can tramadol cause serotonin syndrome even if I’m not taking any other meds?
Yes. Tramadol can cause serotonin syndrome on its own. Unlike other opioids, it directly blocks serotonin reuptake. There are documented cases of people developing full serotonin syndrome after taking only therapeutic doses of tramadol without any other serotonergic drugs. This is especially true in people who are poor metabolizers of CYP2D6, a genetic variation found in about 7% of Caucasians.
How fast does serotonin syndrome develop after taking tramadol?
Symptoms can appear within hours-sometimes as soon as 30 minutes to 2 hours after taking a dose, especially if you’ve recently started or increased the dose. If you’re combining tramadol with another serotonergic drug, symptoms may come on faster. In rare cases, symptoms appear after several days of steady use, particularly in people with slow metabolism.
Is serotonin syndrome from tramadol treatable?
Yes, if caught early. The first step is stopping tramadol immediately. The first-line treatment is cyproheptadine, an antihistamine that blocks serotonin receptors. A typical dose is 12 mg orally, followed by 2 mg every 2 hours if symptoms persist. Benzodiazepines like lorazepam help with agitation and muscle rigidity. In severe cases, patients need ICU care for cooling, IV fluids, and breathing support. When treated within 6 hours, survival rates jump from 22% to over 99%.
What are safer alternatives to tramadol for chronic pain?
For neuropathic pain, gabapentin or pregabalin are often better choices. For general pain, acetaminophen or NSAIDs (if safe for you) are first-line. Tapentadol is an opioid alternative with minimal serotonin activity and a much lower risk of serotonin syndrome. Physical therapy, cognitive behavioral therapy, and non-opioid nerve pain treatments should also be considered. Always discuss alternatives with your doctor before switching.
Should I get tested for CYP2D6 gene status before taking tramadol?
If you’re Caucasian and have a history of unexplained side effects from tramadol, or if you’re being prescribed it for long-term use, yes. Poor metabolizers have a much higher risk of serotonin syndrome. While routine testing isn’t standard yet, major medical centers like Mayo Clinic are already using it in high-risk patients. Ask your doctor if it’s available and appropriate for you.
Why is tramadol still prescribed if it’s so risky?
It’s still used because it works-especially for nerve pain like diabetic neuropathy. About 40-50% of patients get significant relief without side effects, as long as they’re not on other serotonergic drugs. It’s also cheaper than alternatives like tapentadol. But the risk is real and often underestimated. The key is proper screening. Tramadol shouldn’t be a first-line choice for anyone with depression, anxiety, or on antidepressants. It’s a niche tool, not a general painkiller.
15 Comments
Daniel Pate
January 13, 2026 AT 01:19 AM
The real issue isn’t tramadol-it’s the medical system’s obsession with quick pharmacological fixes over root-cause analysis. Serotonin syndrome isn’t a bug, it’s a feature of a healthcare model that treats chemistry like a dial you turn until the pain stops. We’re not addressing why people need opioids in the first place. We’re just swapping one chemical gamble for another.
Amanda Eichstaedt
January 14, 2026 AT 07:28 AM
I had a friend who got serotonin syndrome on tramadol alone. She was on no other meds, just a 50mg daily dose for back pain. She thought the sweating and tremors were ‘just anxiety.’ Took her three days to get diagnosed because the ER doc thought it was a flu. She’s fine now but still has nightmares about the muscle rigidity. This isn’t rare. It’s just ignored. If this was a new cancer drug, the FDA would’ve pulled it off the market years ago.
Jose Mecanico
January 16, 2026 AT 06:54 AM
My cousin was prescribed this after surgery. He didn’t know about the serotonin risk. He’s on Lexapro for depression. He ended up in the hospital with a fever of 103. They didn’t connect the dots until his wife mentioned the tramadol. He’s lucky. Most people don’t make it out of the ICU.
steve ker
January 16, 2026 AT 18:08 PM
Tramadol bad. Doctors dumb. You lucky you alive
Lawrence Jung
January 17, 2026 AT 10:03 AM
People act like this is some new revelation but if you’ve ever studied neuropharmacology you know this was predictable. The FDA knew. Pharma knew. Doctors knew. But nobody wants to admit that the painkiller they’ve been pushing for years is basically a chemical grenade with a pull tab labeled ‘take as needed.’ The real tragedy isn’t the syndrome-it’s that we still treat patients like lab rats until they break.
Monica Puglia
January 17, 2026 AT 17:57 PM
Thank you for this. I’ve been trying to tell my doctor for months that tramadol made me feel ‘off’-like my brain was buzzing. She said it was ‘just adjusting.’ Now I know it was serotonin overload. 🙏 I switched to tapentadol last week and I’m actually sleeping again. No more panic attacks at 3am. If you’re on this and feel weird… listen to your body. It’s not ‘just anxiety.’
Cecelia Alta
January 18, 2026 AT 17:28 PM
Oh my god I can’t believe this is still a thing. My ex got serotonin syndrome from tramadol and a Zoloft and he almost died. The hospital called it a ‘rare side effect’ like it was some kind of lottery win. No. It’s not rare. It’s just that most people don’t survive to tell the story. And now everyone’s acting like this is some shocking discovery when it’s been in the medical journals since 2009. Why are we still prescribing this like it’s Advil? Because it’s cheap. Because insurance won’t cover tapentadol. Because doctors don’t read the damn labels. And because patients are too scared to ask questions. I’m so mad I could scream.
Jay Powers
January 19, 2026 AT 08:31 AM
My dad’s on tramadol for arthritis. He’s 72, on no antidepressants, but he’s a CYP2D6 poor metabolizer. We found out after he had a mild episode-shaking, sweating, confused for hours. We got him tested. He’s switching to gabapentin. This info saved his life. Please, if you’re on tramadol and you’re over 60 or have a family history of weird reactions-ask for the gene test. It’s 2025. We have this tech. Use it.
Craig Wright
January 20, 2026 AT 06:05 AM
It is profoundly concerning that the United States continues to permit the widespread use of tramadol given the well-documented neurochemical risks. In the UK, we have stricter prescribing protocols and mandatory patient counseling. It is not acceptable that patients are left to self-educate on potentially fatal interactions. This is a systemic failure of pharmaceutical regulation.
Rinky Tandon
January 20, 2026 AT 09:24 AM
Tramadol’s serotonergic activity is a Class I pharmacokinetic liability-especially in polymorphic CYP2D6 populations. The clinical implications are non-trivial: increased Vd, prolonged half-life, and elevated active metabolite concentrations. This isn’t anecdotal-it’s biochemically deterministic. Why are we still using a drug with a 7% population-level risk profile as a first-line analgesic? The answer is economic inertia, not medical rationale.
Ben Kono
January 22, 2026 AT 07:42 AM
I took tramadol for a month after my knee surgery. Started feeling like I was vibrating inside. Thought it was stress. Went to urgent care. They didn’t even ask about meds. Told me to take Benadryl. I left and stopped the tramadol that night. Never told anyone. Still don’t know if I had serotonin syndrome or just anxiety. But I’m never taking it again.
Cassie Widders
January 23, 2026 AT 01:27 AM
I didn’t know any of this. I’m on duloxetine for fibromyalgia and my doctor just added tramadol for flare-ups. I’m going to call them tomorrow. Scary stuff.
Darryl Perry
January 24, 2026 AT 09:25 AM
Stop prescribing tramadol. It’s dangerous. End of story.
Alex Fortwengler
January 25, 2026 AT 07:28 AM
Did you know the FDA got paid by opioid manufacturers to downplay tramadol’s risks? And the CYP2D6 testing? They won’t do it because it costs money. This is all a cover-up. Big Pharma doesn’t want you to know you’re a walking time bomb if you’re a poor metabolizer. They’d rather you die quietly than lose profits on tapentadol. Wake up.




Windie Wilson
January 12, 2026 AT 07:16 AM
Oh wow, another ‘your doctor is a monster’ post. I’m sure they just woke up one day and said, ‘Let’s prescribe a drug that might kill people because it’s cheaper than physical therapy.’ 😏